Liver Imaging
For his Wilhelm Conrad Röntgen Honorary Lecture at ECR 2011, Professor Richard Baron MD, from the Radiology Department at the University of Chicago, USA, focused on Detecting liver tumours: the search for the Holy Grail. Why does he compare this aim with that of the medieval knights?

‘The holy grail analogy occurred to me because radiologists – particularly when imaging the liver, wanting to do the best for the patients – have searched for answers without really knowing what they are looking for,’ explained Professor Richard Baron. ‘Similarly, during the Middle Ages, the knights searching for the holy grail actually didn’t know what the grail looked like, they didn’t know where to look for it and they didn’t even know what the grail could do for them if they found it.
‘My lecture focuses on reviewing the dramatic improvements radiologists have made in the past 30 years in their search to ‘do good’ in liver imaging. Similar to the knights, radiologists have been a little narrow in thinking only of what they see in front of them rather than what the patient and clinicians are looking for, or needing. We keep looking to find smaller and smaller tumours on CT. However, if our findings do not affect patient outcome, we are not answering the question of how we can help this patient. We need to define how we can impact on patient care and give information and answers that will help our referring physicians and the patients.
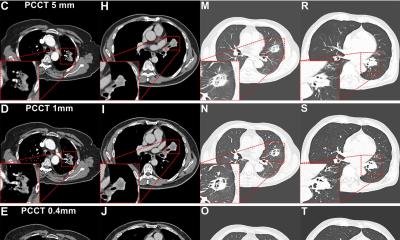
’ Isn’t it important to see the smallest tumours? ‘Yes, of course that’s an example of how we have certainly improved helping patients over recent decades but, in the course of this lecture, I gave some examples where in fact it didn’t make a difference or even may have negatively affected patients. It’s really terrific how we’ve improved our technology, but the process that provided the best gain wasn’t the specific search for a smaller tumour; it was the process of taking the walk. ‘My point is: it is the search that teaches you the most, and how you look around and see what you are seeing and how you are affecting people. When you look at the radiology literature from the very first CT scans in 1978 with very low resolution, until today, you’ve got thousands of papers and every single one says that we see 80-90% of liver tumours. That’s what they said in 1978. The technology got incredibly better and in 1988 the papers still said we see 80-90%.
The technology got even better with helical CT and MR and in 2000 the papers still said we see 80-90% of tumours. It’s part of the process that we are learning how to search better. Obviously we didn’t see 80% of tumours 30 years ago, although the scientific papers would say we did. The researchers were very honest people; they were sincere and serious. It’s just that the process of searching has taught us so much and we’ve learnt how to do it better, including learning the appropriate gold standard to evaluate our efforts.
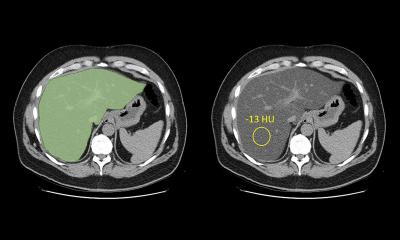
The professor has no doubt that ‘magnetic resonance imaging and the associated contrast agents that have evolved over the last 10 to 15 years for liver imaging have enabled us to detect and characterise tumours in ways we never could have done 20 and 30 years ago. MR is the top modality. It’s been very important to search for the best technology, but that’s just part of the solution we’re looking for. In fact, we also have so many false positives because we see these little things now, so that we may be adversely affecting patient outcome. We may deny them treatment because our techniques are so sensitive that we see meaningless things that are assumed to be significant. ‘We need radiologists who use their cognitive skills to integratethe patients’ clinical data, their history and the current imaging, and we have to be translators who understand the language of imaging, including the nuances of meaning that occurs in different clinical settings, as part of a team to determine the best patient outcome.
Radiologists need to be clinical physicians who understand clinical medicine and can integrate imaging findings and discuss with referring clinicians. Thus I’m looking back to the future: radiologists need to be practicing physicians. We should not lose sight of the important role of a radiologist who understands clinical medicine.’ Most often, a combination of ultrasound and CT are used for liver imaging,’ he explained, ‘Both technologies have greatly improved over the last 20 years and they are really wonderful for staged screening examinations. While MR is probably the most superior technology, it’s the most expensive and there’s limited access to it. We use MR as a problem solver, or in certain specific situations, but having said that, MR is increasingly becoming the standard examination with patients at high risk of liver disease. For patients with hepatitis, for example, who are at risk for hepatocellular carcinoma, we rely very heavily on MR.
Even so, the prevalence of chronic liver disease is so high, we typically screen more with ultrasound and when we suspect more serious problems we move to MR. ‘We occasionally use PET-CT, but not as much as for other parts of the anatomy. Since the liver has so much inherent metabolic activity PET-CT has not become a mainstream modality for the detection of tumours. Occasionally we’ll use it for characterisation but, as far as the liver is concerned, it has not significantly changed the way we approach patients.’ How important is the interdisciplinary approach?
'That’s another analogy to the search for the holy grail: it’s who you interact with and encounter in your processes that can have such a large impact on what you learn, and may even be the key value more than ever finding the grail. So, in my searching for the Holy Grail I`m interacting extensively with hepatologists and surgeons and they teach me what it is they need to know to effect treatment. This is very different from me saying: I want to optimise how many of these lesions I can see when I may not know what they are when I see them.
‘My colleagues have taught me a crucial lesson: sometimes these lesions are important to find and sometimes they aren’t. Without those multidisciplinary interactions we don’t function well as radiologists – for a variety of reasons, not just in the specific case: How do I take care of this one patient? I educate my clinical colleagues as to what radiology and imaging can do for them and their patients and then they educate me as to what they need to learn to effect patient management. Then I can help to determine whether imaging can answer those questions. It’s the communication that’s essential – not just for taking care of patients but also for optimising the lifelong education process.
10.07.2012