Like a torch in the night
No one would think of roaming through unknown territory at night without a torch. Yet, anaesthetists have been doing just that when navigating through peripheral nerve blocks and vessels with a needle. Ultrasound has long been a useful imaging tool in this process. However, so far, this has been a case of the steeper the angle of the needle, the more difficult the ultrasound visualisation.
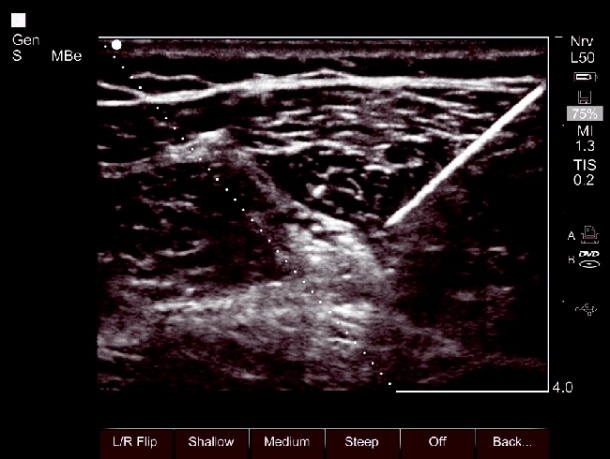

[Bild-1[A new software tool for enhanced needle visualisation can now bring lighten the darkness. SonoSite has spent two years developing an algorithm that can illuminate the needle from three different angles. We spoke with Professor Peter Marhofer of the Clinic for Anaesthetics, Intensive Medicine & Pain Therapy at the Medical University of Vienna, Austria, one of the first users of this new technology,.
Professor Marhofer: ‘The main area of application is currently for deep-lying nerve blocks, which are injected in plane, i.e. along the long axis of the ultrasound transducer. In principle there are two injection procedures: Injecting along the short axis of the ultrasound transducer (out of plane) and along the long axis of the ultrasound transducer (in plane). With the out of plane procedure I can only see the tip of the cannula, with the in plane procedure I can see the cannula tip as well as the shaft.
‘Which procedure is used depends on the individual patient and the type of block. Problems can occur with deep-lying blocks, which are injected in plane. As long as the cannula is guided along flat under the skin, it can be well visualised on the ultrasound image. However, when we go a little deeper we had to do this “blind”, without direct visual control. With the enhanced needle visualisation we now have a procedure that allows us to monitor visually the penetration depth of the needle up to 6cm in case of a 45 degree angle, for instance.’
What types of complications can occur with blind navigation through the blood vessels?
‘First, the needle could puncture an artery, which could lead to a haematoma or an arteriovenous fistula. We also must not underestimate the time delay resulting from the attempt at correct positioning of the cannula. In the case of emergency patients, every second counts.
Does that mean this new technology is also suitable for doctors who are not so experienced?
‘I’d rather consider this a tool for experts. Even with the new technology, the cannula has to be guided into the ultrasound signal to facilitate visualisation. This means that, in the case of a steep angle, we still need a lot of sensitivity to guide the cannula into the correct position. Moreover, the software requires certain handling. There are three different angles at our disposal, which have to be positioned in a right angle to the cannula, i.e. the interaction between man and machine is actually becoming more complex.
What uses might needle visualisation be put to in the future?
‘We’re looking at technology that is still undergoing a lot of further development, so there are still many potential opportunities. I can see a further potential area of application for ultrasound-guided venous puncture and arterial monitoring, and also for new anatomic access, such as central venous access in infants. Administration of local anaesthetic for obese patients is also a topic that is not yet fully understood. We are currently carrying out the first studies in this field. In principle, the procedure has potential benefits anywhere where there is a need for venous or arterial access. I think that ultrasound and enhanced needle visualisation will soon become established worldwide for venous puncture and local anaesthetic blocks. There is no reason to puncture blindly into the vessels when this is actually possible under direct visual control.
17.11.2010