Article • AI in diagnostics
Learn like a human, deduce like a machine
Artificial Intelligence (AI) is like a huge blanket that can cover anything from innocuous chess computers to robots which, depending on your viewpoint, could save, oppress or obliterate humanity. However, not every jar labelled AI contains AI. So what is intelligence and can it be created artificially, synthesised like a nature-identical flavouring substance?

At the Siemens Diagnostik Campus, Dr Martin Hirsch, co-founder and CSO of Ada Health GmbH, explored why the term artificial intelligence is frequently misunderstood and why, nevertheless, this technology has the potential to be a major driver in healthcare.
For some people, machine learning is the computer equivalent of intelligence, but Dr Martin Hirsch begs to differ. ‘For me, first and foremost, intelligence is the ability to generate sensible behaviour in an entirely new situation. An algorithm that iterates a procedure thousands of times and then deduces certain rules from these runs is not necessarily intelligent.’ In other words: intelligence is the ability to generate hypotheses from existing knowledge and, in a next step, to recognise possible courses of action.
While a computer requires innumerable data sets to master a certain procedure reliably, humans in many cases need but a single illustrative example to recognise and understand complex relationships. ‘That’s due to our ability to abstract,’ Hirsch explains. While building knowledge in humans may take much longer than feeding an algorithm with data sets, the brain of a physician, for example, will acquire a deep understanding that can offer a sound solution even in unfamiliar cases.
Recommended article

Article • A look into the crystal ball
Experts debate predictive potential of AI
‘Hello, John? You are about to suffer a heart attack – please come to the hospital immediately!’ Will we, one day, be collected by emergency doctors even before we’re ill? If it was up to some AI experts at Medica, this could be the case – soon. Some obstacles must yet be overcome to achieve perfect AI predictions. Yet, during Medica, some IT experts ventured to gaze into a crystal ball.
Pattern recognition – all the rage in medical applications – might be sufficient to provide a working hypothesis, but never a reliable diagnosis. A pattern recognised by the computer may indeed be due to patient physiology, but it may also be due to poor data, such as image artefacts. ‘When building a decision support system, therefore, we shouldn’t start from square one, but build upon validated scientific knowledge,’ the neuroscientist underlines. Ideally, he says, we use existing knowledge and incorporate insights from pattern recognition. This approach is rather similar to the “human model” where junior physicians first acquire knowledge during their medical school studies and later expand and adapt this knowledge with each day of practical experience.
‘How did you figure this out?’
AI systems will only be able to prevail in a hospital and healthcare system if the machine can explain why it arrived at a certain conclusion
Martin Hirsch
Ada, an AI-based platform developed at Hirsch’s eponymous company, works pretty much according to this pattern. It analyses certain parameters, weighs them and generates a hypothesis from these data, accompanied by a probability score for the validity of the hypothesis. ‘This includes collecting positive and negative evidence, very much like during a differential diagnosis. Ada tries to compare and contrast similar pathologies to differentiate and exclude.’ This procedure is meant to make the ‘thought process’ of the algorithm understandable for the human brain. ‘Transparency is crucial,’ according to Hirsch, because ‘AI systems will only be able to prevail in a hospital and healthcare system if the machine can explain why it arrived at a certain conclusion.’
Currently, the system covers 18,000 disease codes from ICD-10 – a number that is far beyond the capacities of a human physician. ‘Physicians cannot know the entire range of laboratory diagnostics, since the human brain is simply unable to process this degree of complexity,’ Hirsch points out. And, even if the appropriate test is selected, the physician might draw the wrong conclusions from the results. This is where AI comes in to help the physician. A recent study published in the Orphanet Journal of Rare Diseases found that, in 54 percent of the cases investigated, AI could indicate a diagnosis faster than the human physician.
Chatbot anamnesis: digital consultation
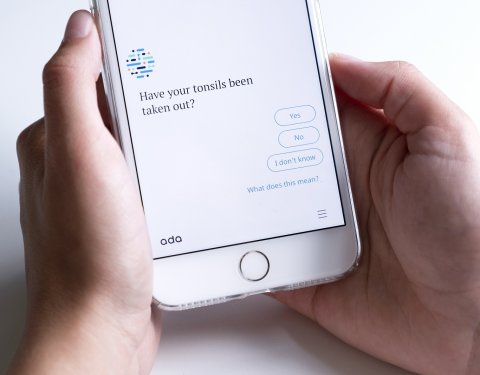
While many physicians are rather wary of chatbots, patients appear to have fewer reservations, as the experience with Ada shows. The patients describe their symptoms to a chatbot, just as they do during a conventional anamnesis, and AI algorithms draw a working hypothesis – a preliminary diagnosis – from these data. ‘To date, we have delivered over 12 million such assessments to more than seven million users,’ says Hirsch, who is convinced that his system meets a real need. The chatbot offers patients something they often miss in their doctor’s office: time. The AI assistant is not under pressure and asks as many questions as necessary to be able to arrive at a conclusion. Moreover, many people find it easier to talk about delicate personal health issues when the counterpart is a machine, rather than a human being. ‘The future healthcare pathway will not start in the physician’s waiting room, but in the patient’s palm. People really do want to find out more about their conditions and possible therapies and this, in my opinion, is the point where AI meets the patients,’ Hirsch says. However, he emphasises that such a system cannot and will not replace the human physician.
These AI developments open many new doors: ‘Such applications can help us structure patient flows in a sensible way,’ Hirsch says, since the recommendations offered by the system can stop people from unnecessary visits to their GP or, even more importantly, to a hospital A&E.
Moreover, the applications have enormous predictive potential, according to Hirsch. When, in early 2019, the number of measles cases in the USA increased massively, AI had seen it coming – six weeks earlier – simply because an unusual high number of users had talked to the chatbots about measles symptoms. Hirsch: ‘Symptom-based epidemiology offers many new possibilities.’
Two further promising areas for AI in healthcare are risk assessment and prevention, Hirsch points out. Even genetic factors can be considered: ‘Genetic data is nothing but probability data. Why then should AI diagnostics, which is also based on probability, not use it?’ Hirsch asks. This means that two patients with identical symptoms might receive different treatments if a genetic test indicates that one of the two has a higher probability for a certain underlying disease.
In developing countries, where specialist physicians are few and far between, AI-based diagnostics could help GPs to treat patients who present with a complex symptom landscape. Even in very basic exams, the developers are confident that AI-based applications can contribute significantly to primary healthcare.
Profile:
Co-founder and Chief Scientific Officer Dr. Martin Hirsch has a Ph.D. in Neuroscience and a Diploma in Physiology. A medical researcher turned serial entrepreneur; Dr Hirsch shifted from theory to innovation after publishing his work on nerve modeling in the scientific journal Nature. His first venture was a nerve modeling program that saved thousands of animals from lab testing. He developed the first version of Ada for doctors and continues to shape the way Ada learns today. Hirsch is a grandson of the celebrated Nobel Laureate Werner Heisenberg.
23.09.2019











