© Prof. Dr. Marco Das
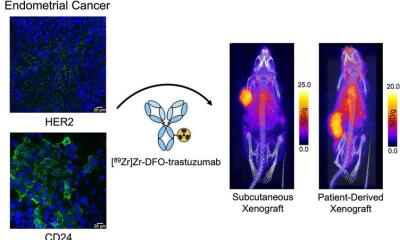
Article • Good-bye “surgery first”
Interventional radiology: out of the shadow and into the light
Using imaging guidance, interventional radiology – a sub-discipline of diagnostic imaging – allows targeted and ultraprecise diagnostic and therapeutic procedures without anesthesia and without large incisions. Nevertheless, surgery continues to be widely considered the procedure of choice, making interventional radiology the Cinderella of the discipline. Professor Dr. Marco Das, Medical Director of the Department of Diagnostic and Interventional Radiology at Helios Klinikum Duisburg, Germany, however, thinks it is high time for Cinderella to take center stage: at Radiologiekongress Ruhr (RKR), he presented new therapy approaches for interventional radiology – and afterwards he kindly took the time to answer HiE's questions.
Interview: Sonja Buske
HiE: Professor Das, which new concepts are currently influencing interventional radiology?
© Prof. Dr. Marco Das
Professor Das: 'The new concepts are primarily results of the current guidelines, particularly regarding hepatocellular carcinoma (HCC) and the treatment of colorectal cancer (CRC). While these concepts are not new, they are playing an increasingly important role in the treatment plans. Particularly ablations such as radio frequency ablation and microwave ablation (MWA) have yielded excellent results with regard to local tumor control proving the idea of “surgery first” obsolete. Rather, the optimum therapy should be selected based on individual tumor site and patient parameters, such as number of lesions, liver function or albumin-bilirubin level. This approach has indeed been integrated in the 2022 BCLC guidelines for HCC and in the 2022 ESMO guidelines for CRC. Moreover, there are new approaches to pain management, for example nerve cryoablation.'
How far have these concepts advanced? Are the methods already being used or are they mere theory?
We have to increase the visibility of the potential of interventional radiology as we can offer a broad range of minimally invasive procedures for a broad range of patients
Marco Das
'The treatment concepts for HCC and CRC are mature. With the traditional focus being on surgery, newer procedures such as MWA were relegated to the sidelines. Today, transarterial chemoembolization (TACE) is more tightly integrated. In this procedure, small particles and chemotherapy materials are applied directly into the blood vessel feeding the tumor. It is also indicated for therapy-refractory HCCs. While cryoneurolysis is still in the early stages, it is a promising alternative for out-patient management of chronic pain.'
With regard to in-patient care, buzzwords are minimal volumes, out-patient care and centralization. Interventional radiology reduces length of stay or doesn’t even require hospital admission at all. What does that mean for your discipline in the clinical context?
'This is indeed a development interventional radiologists should welcome. We have to increase the visibility of the potential of interventional radiology as we can offer a broad range of minimally invasive procedures for a broad range of patients, for example prostate artery embolization, geniculate artery embolization, endovascular treatment of PAD or uterine artery embolization. We could create out-patient services for these procedures but we are currently facing major resource issues, in particular staff shortages.'

© Prof. Dr. Marco Das
What is the current and future role of artificial intelligence (AI) in interventional radiology?
'While everybody is talking about AI, its practical use is still very limited. Regularly, support systems are launched, for example vessel imaging to facilitate embolization. But many hospitals simply don’t have the financial resources to purchase such systems. The potential of AI is huge, down to robotics. AI to support prognoses or non-invasive tumor characterization would be particularly interesting. The future will show which AI approaches will prevail in clinical routine.'
Let’s have a look to the crystal ball: in your opinion, how is – and how should – interventional radiology be changing?
'Interventional radiology will become more visible and use its range of methods to benefit the patients. Research results will increasingly find their way into the guidelines, which means that more and more colleagues will adopt the new knowledge. In short: interventional radiology has a bright future. My personal wish? That colleagues and policy makers alike are open-minded since our healthcare system has to be flexible enough to integrate new methods.'
Profile:
Professor Dr. Marco Das has been Medical Director of the Department of Diagnostic and Interventional Radiology at Helios Klinikum Duisburg, Germany, since 2017. He studied in Düsseldorf and did research at Harvard's Brigham and Women's Hospital. Das has a Master of Business Administration and in 2018 he was appointed Professor (apl) at the University of Düsseldorf.
02.03.2023