Article • Pain Points
MR images can link patient symptoms to pain generators
Have you seen the videos? Perhaps you have read the 20-page paper published in Radiology? At MR 2017 Garmisch you will have the chance to see and hear a live presentation by William Palmer, M.D., Director of Musculoskeletal Radiology & Intervention at Massachusetts General Hospital, a teaching hospital of the Harvard Medical School.

Suddenly in the highly specialized field of spinal interventions, the spotlight is shining on Dr. Palmer, who admits that he is more comfortable performing spinal procedures than taking the stage. At the November, 2016 meeting of the Radiological Society of North America (RSNA), he organized a refresher course on musculoskeletal injections for pain management, and made the keynote presentation in the scientific session on musculoskeletal intervention. Then in December, Radiology published his exhaustive article entitled "How I Do It: Spinal Injections for Pain management." The online publication includes two instructional videos featuring the camera-shy Dr. Palmer.
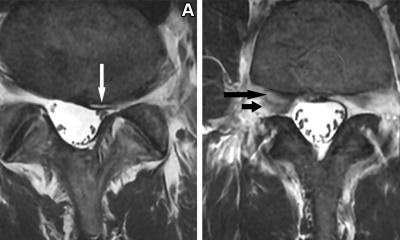
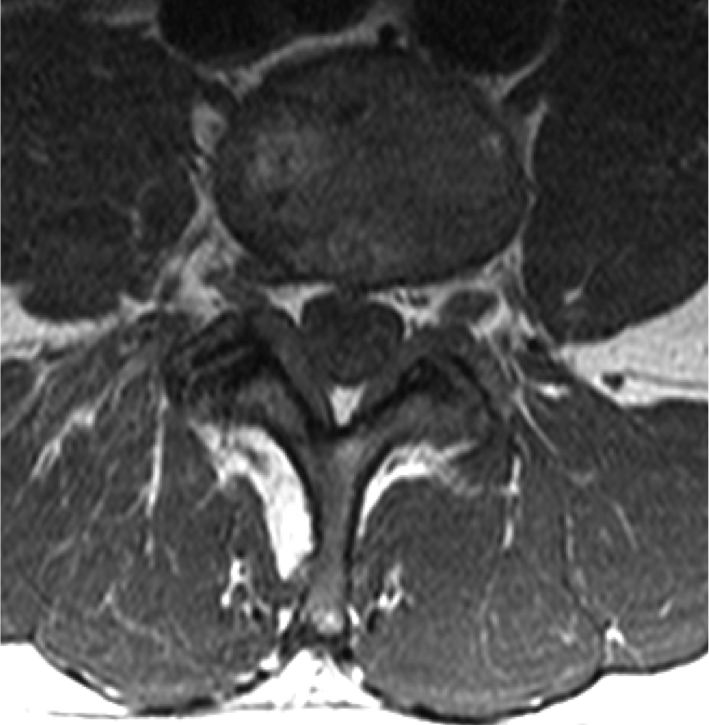
At MR 2017 Garmisch, Dr. Palmer will sharpen his focus on the correlation of patient symptoms with MR imaging findings, the differentiation of active pain generators in the spine from incidental structural abnormalities, and the formulation of a treatment strategy. "Radiologists do a great job addressing these challenges because of our expertise in image interpretation, and our experience with image-guided intervention. We are trained to use imaging to guide the safe and effective placement of needles," he said. MR spine images often show abnormalities in asymptomatic patients, especially older patients who can have numerous findings such as disk degeneration, disk herniation and facet arthritis.
"The challenge is greatest when a patient who has pain also has multiple MR imaging abnormalities. How does the radiologist determine the true pain generator? In the absence of clinical information, the dictated report can become a laundry listing of MR findings without focused conclusions," said Dr. Palmer.
"In spinal intervention and pain management, the radiologist has an opportunity to speak directly with the patient, elicit symptoms, take a targeted inspection of MR images, correlate symptoms with imaging findings, come to a conclusion about the pain generator and decide on the best procedure," he said. “Symptom-imaging correlation can lead to the detection of a subtle but important MR abnormality that was overlooked at the time of the original reporting. Therefore, it can improve diagnostic accuracy and treatment efficacy.”
Anesthesiologists and physiatrists -- the term for Physical Medicine & Rehabilitation Physicians in the United States – also perform pain management injections. Because they are not trained in image interpretation, however, radiologists have the advantage when it comes to symptom – imaging correlation.
Dr. Palmer said his presentation at MR 2017 Garmisch will look at spine MR from the standpoint of corticosteroid injections for pain management. Four factors determine the success of an injection:
- The degree to which the symptoms correlate with imaging findings.
- The degree to which inflammation is the cause of symptoms.
- The degree to which the corticosteroid can be delivered to the inflamed tissue.
- The degree to which the inflammation is reversible.
“My goal is keeping patients out of the operating room," he explained. “Let’s say that a patient with a disk herniation has too much pain for physical therapy and daily activities. That patient might end up in surgery. But if a steroid injection can decrease the inflammation causing pain, the disk herniation might shrink on its own. The patient has a chance to benefit from physical therapy and learn exercises that can help to reduce the severity and duration of pain in the future.”
At MR 2017 Garmisch, Dr. Palmer’s presentation will teach MRI interpretation in the context of symptom – imaging correlation and pain management injections.
Profile:
William Palmer, M.D. is Director of Musculoskeletal Radiology & Intervention at Massachusetts General Hospital (MGH). He received his M.D. from Yale University in 1984, and obtained board certification in Internal Medicine (1987, Hospital of the University of Pennsylvania) as well as Radiology (1991, MGH). He completed fellowship training in MRI at Massachusetts General Hospital (MGH) and joined the MGH radiology staff in 1991. He became its Director of MRI in 1995. Clinical expertise includes sports imaging, arthritis and spine intervention. He oversees 9 MSK radiologists and 5-7 fellows. Currently, he serves as President of the International Skeletal Society, and consultant for the Boston Red Sox, Boston Bruins and New England Patriots.
10.01.2017