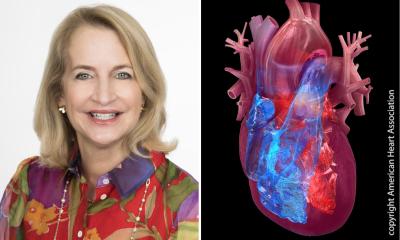
Hybrid approach to treat coronary artery disease
Patients with coronary artery disease -- blockages of the vessels that feed the heart -- can be treated in a number of ways. With their doctor, they decide on the best course of action: surgery, stent placement or medication. Sometimes, a combination of these is the best approach.

Hybrid cardiac revascularization procedures, a combination of bypass and stenting, can reduce the stress of surgery, speeding recovery and potentially improving outcomes.
Dr. Mathew Williams, one of the only physicians in the world trained as both a cardiothoracic surgeon and interventional cardiologist, performs the hybrid procedures at NewYork-Presbyterian Hospital/Columbia University Medical Center.
"Because of my training, I am particularly aware of the benefits and risks of bypass and stenting, and can recommend a customized treatment plan that works best for the patient whether it's one or the other, or both," says Dr. Williams, surgical director of cardiovascular transcatheter therapies at NewYork-Presbyterian Hospital/Columbia University Medical Center and assistant professor of surgery in medicine at Columbia University College of Physicians and Surgeons.
The hybrid approach usually involves minimally invasive surgery using the internal mammary artery to bypass the most important coronary branch, the left anterior descending (LAD). This is followed by a stenting procedure in which tiny metal scaffolds are inserted through an artery in the patient's groin and positioned to prop open the other blocked arteries.
The next step is for both procedures to be performed concurrently. This will be possible in a specially equipped hybrid operating room at the new Vivian and Seymour Milstein Family Heart Center at NewYork-Presbyterian Hospital/Columbia University Medical Center, due to open in the first part of 2010.
Dr. Williams also offers a hybrid approach for other cardiac procedures, including treatment for aneurysms and aortic valve replacement. NewYork-Presbyterian/Columbia also offers hybrid procedures for neurology patients.
"Hybrid procedures are an emerging trend. This is good news for our patients, especially as more physicians receive dual training in surgery and interventional techniques," says Dr. Craig Smith, interim surgeon-in-chief at NewYork-Presbyterian Hospital/Columbia University Medical Center and interim chairman of the Department of Surgery at Columbia University College of Physicians and Surgeons.
"The hybrid approach shows how multidisciplinary collaboration can directly benefit the patient," says Dr. Allan Schwartz, cardiologist-in-chief at NewYork-Presbyterian Hospital/Columbia University Medical Center and the Harold Ames Hatch Professor of Medicine Columbia University College of Physicians and Surgeons at Columbia University College of Physicians and Surgeons.
Dr. Mathew Williams received more than 14 years of medical training, beginning with his medical school training at Columbia University College of Physicians and Surgeons, followed by a residency in general surgery at UCLA. He returned to Columbia for a research fellowship in cardiothoracic surgery. At NewYork-Presbyterian/Columbia, he completed a residency in general surgery, followed by fellowships in cardiothoracic surgery and interventional cardiology.
NewYork-Presbyterian Hospital/Columbia University Medical Center
NewYork-Presbyterian Hospital/Columbia University Medical Center, located in New York City, is one of the leading academic medical centers in the world, comprising the teaching hospital NewYork-Presbyterian and its academic partner, Columbia University College of Physicians and Surgeons. NewYork-Presbyterian/Columbia provides state-of-the-art inpatient, ambulatory and preventive care in all areas of medicine, and is committed to excellence in patient care, research, education and community service. NewYork-Presbyterian, which is among U.S.News & World Report's top 10 hospitals nationally, also comprises NewYork-Presbyterian Hospital/Weill Cornell Medical Center and its academic affiliate, Weill Cornell Medical College.
Source: NewYork-Presbyterian Hospital
Pic: Elisabeth-Krankenhaus, Essen, Germany
15.04.2009