Image source: Mustapha Gambo, Dagin Korona, CC BY-SA 4.0
News • Coronavirus research
How type 1 interferon deficiency hints at severe forms of COVID-19
Which patient will develop a severe form of COVID-19? This is an essential question which must be answered in order to improve the individual management and the prognosis of these patients.
In a publication in the journal Science, teams from the Assistance publique – Hôpitaux de Paris (AP-HP), Inserm, Université de Paris, Institut Pasteur and Institut Imagine describe a unique and unexpected immunological phenotype in severe and critical patients, consisting of a severely impaired type I interferon (IFN) response, associated with persistent blood viral load and an excessive inflammatory response.
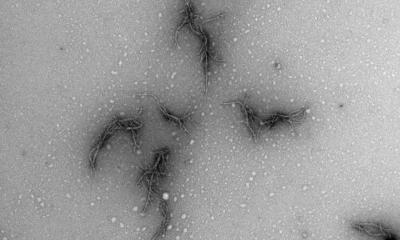
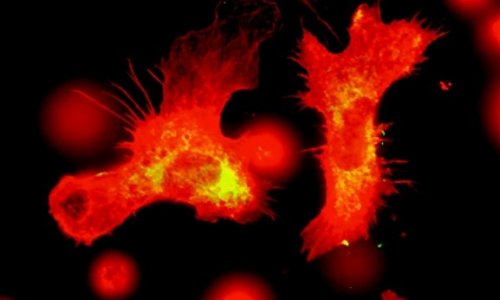
About 5% of people with COVID-19 progress to a severe or critical form, including severe pneumonia, which turns into acute respiratory distress syndrome (ARDS). These forms sometimes occur at the beginning of the disease, clinical observations generally describe its progression in two stages, starting with a mild to moderate form, followed by respiratory worsening 9 to 12 days after the appearance of the first symptoms. This sudden development suggests a deregulation of the host's inflammatory response. A growing body of evidence suggests that this worsening is caused by a sharp increase in cytokines. This runaway inflammatory response is correlated with massive infiltration into the lungs of innate immune cells, namely neutrophils and monocytes, creating lung damage and ARDS.
Recommended article
News • Deadly mechanism uncovered
Inside COVID-19's 'cytokine storm'
Leading immunologists in Japan are proposing a possible molecular mechanism that causes massive release of proinflammatory cytokines, or a cytokine storm, leading to the acute respiratory distress syndrome (ARDS) in COVID-19 patients. Their suggestions, published in the journal Immunity, are based on recent findings that explain how SARS-CoV-2 enters human cells.
Because of similarities to a genetic disease leading to a comparable pulmonary pathology, researchers initially assumed an excessive production of IFN, a marker response to infections. However in seriously ill patients, the teams show that both production and activity of type I IFNs are greatly reduced in the most severe forms of COVID-19. Added to this is a persistent viral load in the blood, testifying to the poor control of viral replication by the immune system of patients and leading to the runaway of an ineffective and pathological inflammatory response. Inflammation, caused by the transcription factor NF-kB, also leads to an increase in the production and signaling of tumor necrosis factor (TNF) -alpha and interleukin IL-6, a pro-inflammatory cytokine.
Recommended article

News • Coping with Covid-19
How France handles the coronavirus pandemic
The first case of the new coronavirus infection was reported on the 24th January. The strategy taken by the French to stem the spread of the virus and relieve the pressure on the health service may seem draconian to some, but many feel that it is either not strong enough and/or too long in coming because it is only recently that the borders have finally been closed.
This weak signature of type I IFN differs from the response induced by other respiratory viruses such as human syncitial respiratory virus or influenza A virus, both of which are characterized by high production of type I IFN.
The study also reveals that low levels of IFN type 1 in plasma precede the clinical worsening of patients and their transfer to intensive care. Circulating IFN type 1 levels could be used to stage of the disease, with the lowest levels seen in the most severe patients. These results suggest that in SARS-CoV-2 infection, the production of type I IFN is slowed down in the infected host, which could explain the more frequent severe forms in individuals with low production of this cytokine, such as the elderly or those with co-morbidities. Therefore, type I IFN deficiency could be a signature of severe forms of COVID-19 and could help identify a high-risk population.
These results further suggest that administration of IFN-alpha in combination with anti-inflammatory therapy targeting IL-6 or TNF-α, or corticosteroids such as dexamethasone, in the most severe patients may be a possible therapeutic pathway to stop severe forms of COVID-19.
Source: Université de Paris
16.07.2020