© Christian Morawe/Universitätsmedizin Magdeburg
Article • Focused ultrasound
Histotripsy: fighting tumors with microbubbles
Interview with Prof. Maciej Pech, Director of the Department of Radiology and Nuclear Medicine at University Hospital Magdeburg.
Focused ultrasound waves create microbubbles in a fluid – a phenomenon called cavitation. In a current study, this process is used to destroy liver tumors and metastases. In this Medica-tradefair.com interview, Prof. Maciej Pech talks about testing cavitation events generated during histotripsy, explains the process, and reveals its advantages.
Prof. Pech, what is the purpose of the #HOPE4LIVER study?
Prof. Maciej Pech: This phase I clinical trial investigates the safety and efficacy of the histotripsy method in the treatment of liver lesions. This includes primary and metastatic liver tumors.
What is histotripsy?
Histotripsy is a method based on sound waves that induce cavitation. During a low-pressure cycle, high-intensity ultrasound waves lead to the formation of small vacuum bubbles or cavities in the liquid. When these bubbles reach a volume at which they can no longer absorb the energy, they implode when subjected to higher pressure. The bubbles form within a narrow region via the superposition of ultrasonic waves and destroy tumor cells at the cellular organelle level.
After creating the treatment plan, a robotic arm performs point-by-point ablation in the targeted tumor area and respective clearance zone. This is a very precise maneuver as the ultrasound is focused with millimeter-precision.
How long has this technique been around?
The method has been used in experiments and in research laboratories for the past 15 years, but clinical trials are just now underway. The forerunners of this technique include lithotripsy, a procedure that applies shock waves to break up stones in the kidney and parts of the ureter, or thermal ablation using focused ultrasound. Histotripsy is non-invasive and does not produce heat in the tissue. Cavitation destroys the targeted area completely.
Where can the technique be used?
Once the accuracy and safety of this technique has been proven, I could envision its application to treat the affected lymph nodes, bladder tumors, and kidney cancers
Maciej Pech
In theory, you can use the method anywhere in the body for all types of tissues that can be radiated with focused ultrasound. However, there are some physical limitations. It is difficult to use the process behind a bone because the ultrasound is reflected off the structure. It is also not an ideal technique for air-filled organs.
Once the accuracy and safety of this technique has been proven, I could envision its application to treat the affected lymph nodes, bladder tumors, and kidney cancers.
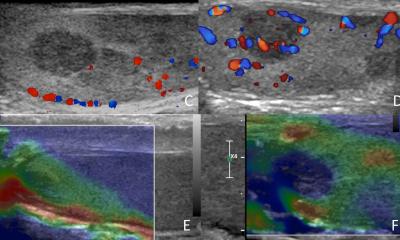
Does imaging accompany the procedure?
Imaging is primarily used for treatment planning during which the tumor is highlighted using the ultrasound image. The liver ultrasound scan is available during the exam. It does not have the same quality as we see in primary diagnostics, but you can detect the bubble cloud shape in the tumor, giving you direct control over the sound waves to trigger cavitation in the targeted area. This facilitates online monitoring during the procedure and provides added visualization and safety.
What are the advantages of this method?
It is a non-invasive technique, which means it carries no risk of infection and there is no need to tend to or monitor wounds. That is why this is a conceivable outpatient treatment that does not require an overnight stay at the hospital. The patient could simply return to the hospital the next day for a checkup if he lives near the facility.
Are there any known risks?
So far, we are not aware of any. In theory, there is always the risk of poor planning, or that the energy is applied at the wrong spot. This is why visual tracking during the procedure is key. The robotic arm is far more accurate in applying the energy than humans.
Another risk is that the patient could make involuntary movements by breathing or coughing, for example. You would have to stop and reschedule the intervention immediately, which is why anesthesia is used for the purpose of this study. However, one might also consider simple sedation in the future.
What is next for the study?
It is currently a classic phase I clinical trial that seeks to evaluate the safety and efficacy of the process. In the next phase, the mechanism of histotripsy would be tested in a randomized setting against an established method. This could be thermal ablation, radiofrequency ablation, or stereotactic radiation therapy.
The interview was conducted by Timo Roth and translated from German by Elena O'Meara.
17.11.2021