Image source: Heraeus
Sponsored • PJI risk mitigation
Arthroplasty: Avoiding infection and revisions in high-risk patients
The main goal of arthroplasty is to relieve pain, improve and restore joint function and recover quality of life. Periprosthetic joint infection (PJI) remains a complication that has to be taken seriously for those receiving arthroplasty surgery. The risk of infection for those receiving primary resection is up to 2%, rising to up to 5% for those undergoing revision.
There are many reasons why PJI can occur; it is sometimes down to the patient themselves. Patients each possess their own risk factors, which can increase the likelihood of developing an infection, both for those receiving primary and revision arthroplasty. For every ten patients over the age of 65, six will display at least two risk factors for infection. The latest studies suggest that individual risks or complications that can lead to PJI should be examined in relation to defined patient profiles. They provide initial findings that can be used, in the future, to develop promising arthroplasty treatment strategies that are geared towards different patients.
Approaches to arthroplasty surgery should be tailored to the patient
In clinical practice today, you can find different approaches aimed at avoiding complications and revisions in arthroplasty, such as PJI, periprosthetic fractures, dislocations and aseptic loosening, in an effective manner. What these all have in common is that the patient, with their individual risk profile, should be considered in a situational manner to include the following in their treatment plan: the patient’s current comorbidities and the surgery-associated risks.
Recommended article

Sponsored • Orthopaedics
Periprosthetic joint infection: a complex issue
Periprosthetic joint infection (PJI) can be an enormous challenge for orthopaedists and trauma surgeons. Antibiotic-loaded bone cement is an important element in a prevention strategy.
Taking the patient-related risk factors into consideration
For example, patients that suffer from risk factors such as obesity, diabetes or cardiovascular diseases have a disproportionate risk of developing acute or chronic infections in the area surrounding the joint prosthesis following arthroplasty surgery. Many studies have shown there is a correlation between an increased Body-Mass-Index (BMI) and an increased risk of infection. Compared to non-obese patients, the rate of polymicrobial infection is higher in obese patients (60.3% compared to 33.3%, p<0.001). Uncontrolled diabetes is a known separate risk factor in the development of periprosthetic infection. For patients suffering from cardiovascular diseases, chronic blood vessel damage and medicines that influence clotting and thrombocyte function can all increase susceptibility to infection.
As many of these risk factors cannot be reduced in the short-term before surgery, targeted infection prophylaxis strategies are vital to help prevent infection. This also goes hand in hand with the decision to use antibiotic-loaded bone cement when fixing prostheses.
Indication-based treatment strategy: risk classification in primary arthroplasty
A patient’s individual comorbidities have a considerable influence on their risk of infection and should be considered when selecting the optimal treatment algorithm. The first steps when deciding on the treatment and therapy to be deployed are to identify the patient’s comorbidities. When possible, this will go hand-in-hand with preoperative comorbidity optimisation.
Classifying patients at risk of infection, even for primary procedures
To prevent periprosthetic infection in patients at risk of infection in an effective manner, including during primary arthroplasty, a definition should be established to identify which patients can be classified as being at risk of infection. One approach from Spain takes the combination of a number of different risk factors into account, including comorbidities, the patient’s various pre-existing conditions and surgery-related risks. For example, in elective primary hip arthroplasty (TEP) and hip arthroplasty following trauma, a patient is classified as being at-risk if they have a combination of at least three risk factors, whereas for elective primary knee TEP, patients are classified as at-risk if they show at least two risk factors.
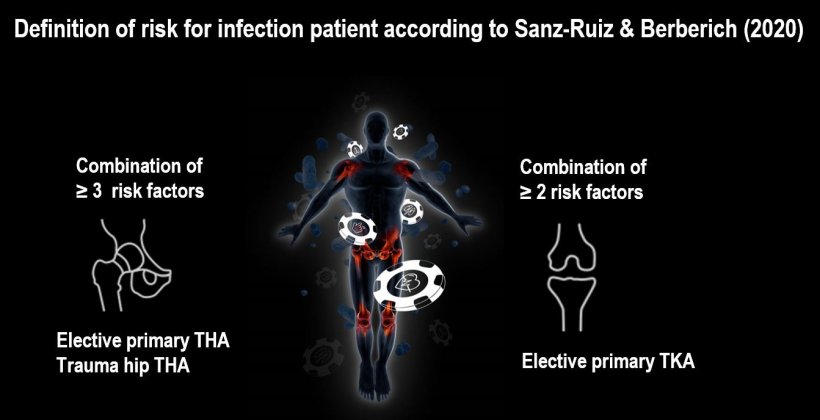
Image source: Heraeus
Infection reduction with dual antibiotic-loaded bone cement
It has been shown that for patients at risk of infection with a selected risk profile, the risk of developing PJI following primary hip or knee arthroplasty surgery can be additionally reduced through the application of dual antibiotic-loaded bone cement. A further report from Spain has shown a PJI reduction of 34% from 3.7% to 2.45% for primary hip and knee arthroplasty in high-risk patients through the use of a dual antibiotic-loaded bone cement, compared to the use of a single antibiotic-loaded bone cement.
Source: Heraeus
08.08.2022