Image source: Adobe Stock/zapp2photo
News • High-glade glioma research
Understanding why deadly brain cancer comes back
A new study, by a global team including Leeds experts, has found that in response to treatment, high-grade gliomas appear to remodel the surrounding brain environment, potentially creating interactions with nearby neurons and immune cells in ways that protect the tumour cells and hide them from the body’s defences.
The findings are now published in Cell journal.
The team also found that lower-grade tumours often develop a new mutation that allows the cells to start dividing more rapidly, potentially catapulting them into a higher-grade form.
This study has allowed us to gain unprecedented insight into how these deadly tumours progress, and ways that we might finally be able to stop them
Lucy Stead
Glioma brain tumours are rare, but a diagnosis is devastating because there is currently no cure. Low-grade gliomas have a better survival rate than, but often progress to high-grade gliomas. More than 90% of patients with high-grade tumours die within five years. Current treatments include surgery, radiation therapy and chemotherapy. The findings indicate that new drugs are needed to supplement these. Dr Lucy Stead, Associate Professor of Brain Cancer Biology in Leeds’ School of Medicine, and the lead UK academic for the study, said: “The brain is a hugely complex organ made up of lots of different types of cells, and brain tumours are equally diverse and complicated. Learning from patient tissue is the best way to cure the patient disease. This study, which required a global effort to acquire enough glioma samples to adequately power it, has allowed us to gain unprecedented insight into how these deadly tumours progress, and ways that we might finally be able to stop them.”
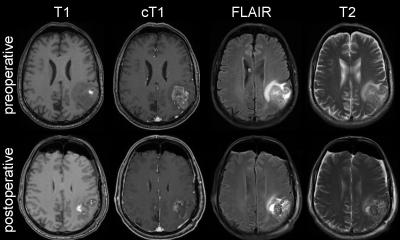
The researchers are investigating why gliomas progress to a higher-grade form, and why they survive and continue to grow after treatment. They collected multiple samples of gliomas over time, as they transitioned from low-to-high grade, and before and after treatment. They then looked at how the cells changed and adapted to see if they can find ways to stop them, using novel drugs. The mutation and previously unknown cellular interactions could now be targeted with novel drugs that stop the tumour cells progressing and adapting to treatment. In this way the study has opened new avenues of research that may yield more effective drugs to offer patients.
The research was led by Jackson Laboratory (JAX) Florine Deschenes Roux Chair Professor and senior author Dr Roel Verhaak, and Postdoctoral Associate and Jane Coffins Childs fellow first author Dr Frederick Varn. Dr Varn said: “By analyzing genetic and transcriptional data from this large cohort of patients, we are beginning to appreciate how tumours are changing to adapt to standard-of-care therapy. This study has made it clear that not every tumour changes in the same way. Knowing this is going to allow us to develop therapies that are better tailored towards each patient’s disease in the future.”
Dr Verhaak said: “The GLASS project has built tremendous momentum and is just getting started. We are well underway to tripling our patient cohort and datasets. We are poised to comprehensively dissect the process of resistance and make important progress towards better outcomes for patients with a glioma.”
Source: University of Leeds
23.08.2022