Getting to the heart of things
Not only is heart failure one of the single biggest causes of morbidity and mortality in man, but the incidence of the condition is steadily increasing. Rising to this challenge, innovative medical diagnostic techniques with ever greater performance are constantly being introduced so that early, unambiguous detection of the underlying condition is now possible, enabling the prompt initiation of targeted therapies.
Some 14 million people in Europe currently suffer from heart failure (HF) with the number predicted to increase to no fewer than 30 million by 2020. The medical impact of HF is huge -- in particular, the condition is associated with high mortality. After the first incident of cardiac decompensation, as many as around 40% of patients will die within one year. Of those who survive the first year only one third will actually live longer than a further five years. The social impact of HF is also significant and is understandably associated with immense costs, which put an additional financial strain on already tight healthcare budgets.
Thus the early detection and adequate treatment of cardiac diseases is of utmost importance.
The latest developments in imaging and in vitro diagnostics offer new opportunities for detecting HF not only much earlier but also with great precision.
Echocardiography
Ultrasound examination of the heart, i.e. echocardiography, is the basic imaging technology (and also the least expensive) in cardiology and, in the vast majority of patients, plays the role of a ‘gate-keeper’ controlling access to eventual additional diagnostic procedures that may be needed. The latest echocardiography systems now enable real-time 3-D full-volume images of the beating heart so that the heart can be imaged to depict the whole organ easily and rapidly, not just in 2-D, but in full volumes. They can display, analyse and capture the heart in full in a single heartbeat. These echocardiography results are the prerequisite for other, more expensive examinations, which may be necessary.
Echocardiography is widely available in hospitals and in nearly all cardiology practices, while newer imaging technologies, e.g. cardiac CT or MRI, which may be indicated for further diagnostic investigation, are in general found mostly in larger facilities.
Cardiac MRI
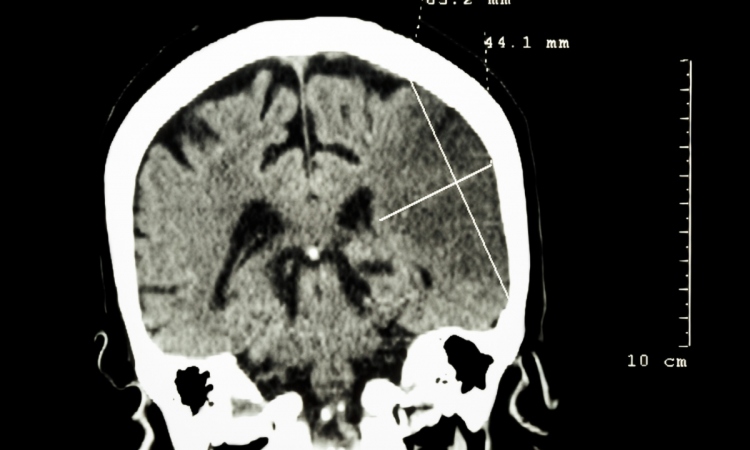
One of the most recent imaging techniques used to analyse the heart is magnetic resonance imaging (MRI), which, in addition to the fact that it does not involve the use of ionising radiation, in contrast to CT, provides a comprehensive (and highly accurate) assessment of the heart. Cardiac magnetic resonance imaging (CMR) can also yield penetrating insights into the underlying pathology of a failing heart. Known as the gold standard for the assessment of cardiac function, cardiac MRI is used as the most accurate non-invasive tool to measure parameters like ejection fraction, based on which patients may get a drug therapy alone or even devices implanted (such as pacemakers or defibrillators). CMR also provides a special imaging approach for the visualisation of even the smallest scars in the myocardium [Fig.1], which is important since the presence and extent of myocardial scarring is a major risk factor for sudden cardiac death. It has been shown in many recent clinical studies, that CMR allows accurate assessment of myocardial scar formation with extremely high diagnostic accuracy. CMR is the best non-invasive approach to address this important clinical question. For this reason, a growing number of cardiologists are using the procedure to identify patients with HF who are in need of an implantable defibrillator, which protects against cardiac arrest through targeted shock delivery.
Until recently, because of the high magnetic fields used in the technique, CMR was contraindicated in patients with pacemakers. Thanks to cooperative development between the manufacturers of MRI systems on the one hand and pacemaker devices on the other, MRI-conditional pacemakers∗ are beginning to become available (e.g. from Medtronic). Since MRI scanners may cause traditional pacemakers to misinterpret MRI-generated electrical noise and withhold pacing therapy or deliver unnecessary pacing therapy, the new generation of pacemakers includes features that set the device into an appropriate mode for the MRI environment. Such pacemakers also include hardware modifications to the device and leads that are designed to reduce or eliminate the influence of the MRI environment.
At the practical level, MR examinations of the heart are no longer complicated or time-consuming. In general, a CMR examination for the evaluation of cardiac anatomy, function and scarring can now be carried out within 20 minutes.
∗ “MR-conditional” is a term used to indicate that a device may be used in the MRI environment under certain conditions, such as a particular type of MRI scanner and scanner settings.
Coronary vessels in view: cardiac CT
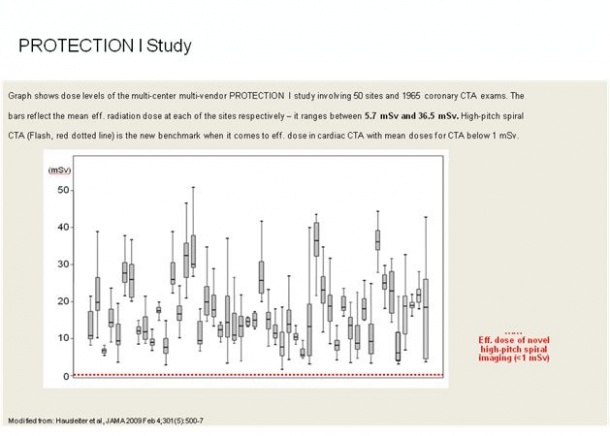
Computed tomography (CT) has long had a valuable role in early disease detection over the years. Steady technological development over the years means that the latest generation of CT scanners can now carry out coronary CT angiography (CTA) with significantly reduced radiation dose [Fig.2] in daily clinical routine. The most recent innovation, namely the use of ECG-triggered high-pitch spiral data acquisition using dual source CT as implemented in the SOMATOM Definition Flash system from Siemens can carry out CTAs at radiation doses as low as below 1 mSv, which is less than in conventional coronary angiography. [(By comparison, one mSv is less than half of the annual natural background radiation on earth, to which everyone is exposed).
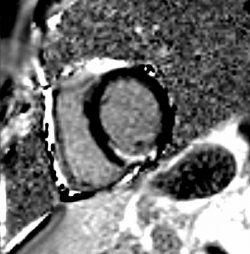
Unlike a cardiac catheter examination, CT can not only visualise the coronary lumen, but also display deposits (plaque) in the coronary wall. The calcium load of the coronary vessels (known as the Calcium Score) can be quantified in CT without the use of contrast agent. An age-adapted increased calcium load of the coronary arteries is as much a risk factor as smoking or increased cholesterol. Recent studies have shown that high Calcium Score can modify predicted risk obtained from traditional risk stratification tools (e.g. Framingham Risk Score) alone, especially among patients in the intermediate risk category in whom clinical decision making is most uncertain. In practice, using the latest technology coronary CT examinations can be carried out in less than a second and are therefore especially useful in patients with cardiac arrhythmias and older patients, since the short time-span means that the patients can breathe normally [Fig. 3]. The procedure is also optimal and time-efficient for the physician, since now a single mouse click generates a meaningful image and thus saves up to 17 manual processing steps, where previously lengthy image processing was necessary. Of course, such innovations inevitably have their price, with, for example, large medical installations such as MRI or CT scanners costing up to 2 million Euros. However, it is important to realise that the appropriate use of these new technologies may save overall health care expenditure over the long term: thanks to better diagnostics, treatment can be initiated much sooner. As a consequence, quality of life can be preserved and loss of productivity avoided.
Nuclear Cardiology examinations are widely available and well-established in patients with suspicion of hemodynamically relevant CAD. Myocardial SPECT scintigraphy enables ischemia detection and relevance by examining left-ventricular function as well as myocardial perfusion at rest and under vasodilator stress (adenosine/dipyridamole). Fixed perfusion defects (at rest and stress) allow judgement about myocardial viability.
PET/CT myocardial perfusion imaging (MPI) using short lived radiopharmaceuticals such as Rubidium-821 (82Rb) or Nitrogen-13 ammonia (13NH3) has been shown to have high sensitivity and specificity for diagnosis and characterisation of coronary artery disease (CAD). The quantitative nature of PET and its dynamic imaging capability enable computation of myocardial blood flow (MBF) during rest and peak stress and calculation of coronary flow reserve (CFR). This quantitative approach improves the evaluation of myocardial ischemia and functional estimation of coronary stenosis as well as the characterisation of diffuse or triple vessel disease.
Minimally invasive therapy: intervention instead of surgery
Some underlying diseases of HF - such as severe valvular disease - often require therapeutic interventions beyond drug therapy involving cardiologists and surgeons at the same time. The cardiac cath lab of the future is already being implemented in some centres in the so-called Hybrid-ORs which, by bringing together the features of the surgical room with those of a cath lab, making possible innovative therapies, such as in the treatment of severe aortic valve stenosis. Until now, valve replacement by open-heart surgery was the recommended therapy approach in these cases, but in many elderly patients with concomitant diseases this can be too risky. Interventional implantation of an aortic valve prosthesis has become an alternative in such patients, and can give rise to rapid improvement of cardiac parameters. In this procedure the valve prosthesis is placed via the femoral artery or, if this is not possible, by a small incision in the apex of the heart. Such a ‘minimally invasive’ intervention puts much less stress on the patient than an open heart operation. Overall, providing technical equipment needed to accommodate multiple specialties in one lab may allow for better quality of care as well as better time and cost efficiency for both the patient and institution.
Biomarkers
The presence and course of HF can also be assessed using in vitro lab tests, through the use of new biomarkers which, especially in emergency care, can influence and support clinical decisions. In HF the use of circulating B-Natriuretic peptide (BNP) is particularly relevant, since the level of this biomarker is a good indicator of the degree to which the cardiac function is impaired. BNP is used both for initial diagnosis and for therapy monitoring. Recent studies have shown that in the presence of other risk factors and known HF, BNP has also a prognostic value, i.e. patients with BNP above a certain level will be candidates for more aggressive risk management. In many patients, a heart attack is the direct cause of cardiac insufficiency, so fast detection of a myocardial infarction (MI) is extremely important in order to prevent severe myocardial damage and subsequent HF. To do this, more and more emergency rooms routinely use high sensitive Troponin I tests as an early and precise indicator of MI . Significant time can be saved in this way so that the recommended therapy, such as the re-opening of the occluded coronary artery by cardiac catheterisation, can be initiated immediately. Since for every second that the coronary artery remains occluded muscle cells will die (in the classical dictum ‘time is muscle’), rapid intervention is of course vital.
Author: O. Ekinci, MD
References
1. Assomull et al. Cardiovascular Magnetic Resonance, Fibrosis, and Prognosis in Dilated Cardiomyopathy. J Am Coll Cardiol 2006; 48: 1977-85.
2. Kim HW et al. Cardiovascular magnetic resonance in patients with myocardial infarction: current and emerging applications. J Am Coll Cardiol 2009 Dec 29; 55(1):1-16 Page 5/6
3. Achenbach et. al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010 Feb; 31(3):340-6
4. Polonsky TS et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010 Apr 28; 303(16):1610-6.
5. McKie et al. The Prognostic Value of N-Terminal Pro–B-Type Natriuretic Peptide for Death and Cardiovascular Events in Healthy Normal and Stage A/B Heart Failure Subjects. J Am Coll Cardiol. 2010; 55:2140–7.
6. Bonaca M et al. Prospective Evaluation of the Prognostic Implications of Improved Assay Performance With a Sensitive Assay for Cardiac Troponin I. J Am CollCardiol. 2010; 55:2118–24
20.08.2010