Artificial insemination
France: The country’s first ‘saviour sibling’ is a ‘double-hope baby’
Annick Chapoy reports from Paris
The birth, in France, of its first baby to be conceived by artificial insemination on top of the selection of an embryo based on its blood, has sent new flames into the hot parliamentary debate over the reform of bioethics law.


The child’s deliberate embryonic selection rested on it not having the gene for beta thalasaemia, and its birth potential to help cure beta-thalasaemia suffered by two older siblings. Theoretically, the use of ‘saviour siblings’ has been allowed since 2006, when the 2004 Bioethics Law and associated decrees was passed. The USA has utilised this for about ten years, but such a birth is rare in Europe – and, depending on the results of a current debate, might become even rarer in France.
Umut-Talha -- a name meaning 'our hope' in Turkish – entered life this February in Clamart, south-west of Paris. He weighed 3.65kg and was pronounced ‘very healthy’. His birth resulted from in vitro fertilisation after a double pre-implant genetic diagnosis that enabled doctors to choose an embryo that would not carry the disorder beta-thalasaemia, and whose blood and tissue would be compatible with that of his brother and sister. This type of technique was legalised in France with the Bioethics Law of 2004, but is still the source of great controversy in the public.
It is the first successful birth resulting from this type of pregnancy in the country. The practice is legal in numerous other European countries, including Spain and Belgium where, in 2005, the first two 'medicine babies' in Europe were born. The first birth of this type took place in the USA in 2000.
France’s first so-called ‘saviour sibling’ was born to parents of Turkish origin and he was conceived under circumstances that would have been unthinkable only a generation ago. Umut Talha’s parents had approached the hospital in Clamart just over a year ago. They had a serious problem -- their two youngsters were both afflicted with the inherited blood disorder beta thalasaemia, which requires monthly blood transfusions. The parents knew the hospital was one of only three in France that was developing a treatment for their children's illness.
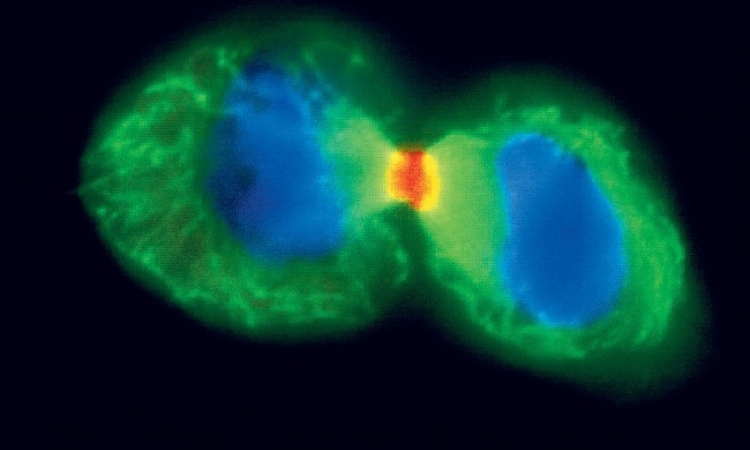
An embryo was screened and genetically selected from an original group of 12 embryos. It was chosen to ensure it did not carry the Beta thalasaemia gene and also due to its compatibility with the sick siblings. Besides selecting an offspring that would be spared from the disorder, the parents hoped their future baby could also become a donor of the right kind of treatment cells.
Born disorder-free, the baby’s cells also proved compatible with his two-year-old sister. Doctors feel confident that she will be cured with the cells from his discarded umbilical cord, and her monthly blood transfusions will be discontinued.
The family have since returned to their home in southern France, but plan to return to Clamart to undergo the same procedure to cure their other child, Umut’s four-year-old brother.
Following his birth, French newspapers spread ‘Medicine baby’ headlines across their pages. However, Professor René Frydman, a fertility pioneer and the ‘medical father’ of the first French test-tube baby in 1982, oversaw Umut’s case, said he preferred the term ‘double-hope baby’.
‘Medicine baby is a media term invented by people who are against this kind of procedure,’ said Prof. Frydman. In English-speaking countries, the terms ‘donor baby’ and ‘saviour sibling’ have been widely used in the media.
Umut certainly presents a double hope for his parents: the hope of having a new, healthy baby, and the hope of curing one of their sick children.
However, other scientists, religious groups and parents beg to differ. The issue of saviour babies has raised complex ethical debates, and renewed fears of a move towards ‘designer babies’, or babies whose traits – e.g. intelligence, eye-colour and height – have been predetermined.
Thus, Umut’s birth has raised questions among medical, political as well as religious circles in France. Christine Boutin, President of the Christian-Democratic party, denounced an ‘instrumentalisation of the human being, conceived in the sole purpose of being used’, while the head of the Bishop’s Conference said he was ‘totally opposed to a procedure by which somebody is being used exclusively to serve somebody else’.
The timing of Umut's birth was also significantly timely -- just as the very law that allows for cases such as this to be revised. Observers say that the existing legislation guiding biotechnology in France might be tightened and restrict research in certain fields, including stem cells.
The country’s standing bioethics law allows for cases like Umut’s. In fact, the government has earmarked €800,000 per year for Clamart to practice and develop the procedure.
Nonetheless, Prof. Frydman and colleagues say a lot more needs to be done, complaining of endless hurdles to launch further research and access funds. They regret that France has started a decade after the USA and that the government is still reluctant to give them full backing.
18.04.2011