Image source: National Cancer Institute (NIH), Cecil Fox
News • Groundwork for new treatments
Fibrosis a prognostic biomarker for HER2-negative breast cancer
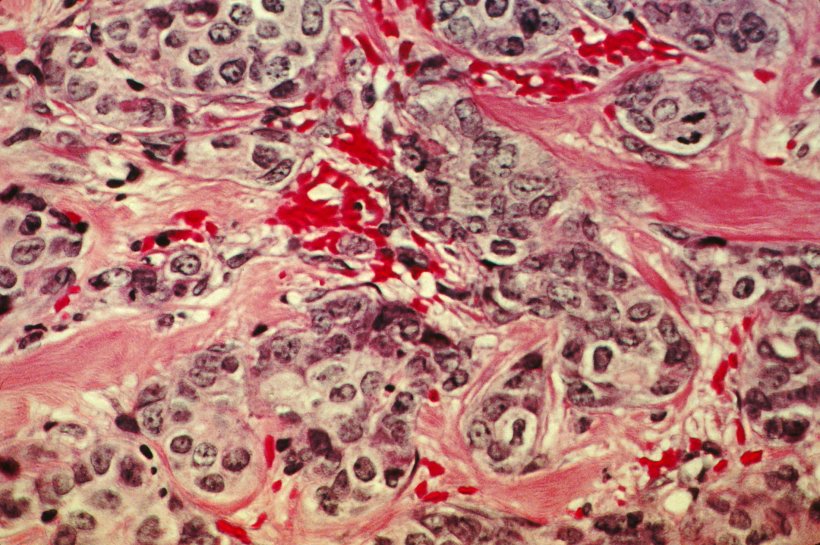
The most common breast cancer is HER2-negative, so called because it has low amounts of one of the proteins that contribute to tumor cell growth, HER2.
Despite this common trait, the development of HER2-negative cancers varies among patients, so one goal is to be able to classify tumors in more detail and thus determine the best treatment for each case.
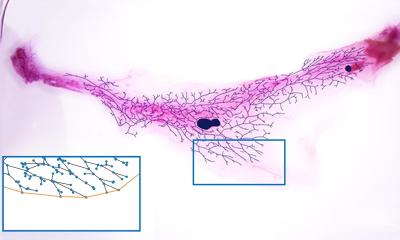
The Breast Cancer Clinical Research Unit at the Spanish National Cancer Research Center (CNIO) confirms that a feature that helps predict the evolution of the disease is the rigidity of the substances that give structure and support to the tumor cells – the so-called extracellular matrix –. This causes a hardening, or fibrosis, of the tumor tissue, which conditions the way in which the cells spread. The CNIO team, led by Miguel Ángel Quintela, finds in a new study published in Clinical Cancer Research that the prognosis is worse when fibrosis is present.
This is the first time that a drug with antifibrotic activity has demonstrated activity, but also very potent one, in cancer
Miguel Ángel Quintela
The relationship of fibrosis of the extracellular matrix with tumors and, in breast cancer, with the propensity to metastasis had already been observed. But now “for the first time in a clinical study, the role of fibrosis as a very adverse negative prognostic factor has been confirmed,” Quintela says.
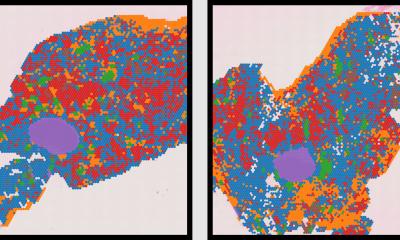
The study evaluates a new test called MeCo Score, which analyzes the activity of about 1,000 genes in early-stage HER2-negative breast tumor tissues, and focuses specifically on genes whose expression is related to fibrosis. The test – developed by the company MeCo Diagnostics, a spin-off of the University of Arizona, based on the work of the study’s first author, Gus Mouneimne – establishes a scale for the results. The study has verified that the higher the score, the greater the presence of fibrosis and the greater the likelihood of relapse and/or metastasis.
MeCo Score also contemplates an innovative treatment option. Its results indicate the effectiveness that supplementing conventional chemotherapy with a drug currently used against idiopathic pulmonary fibrosis, nintedanib, can have on these tumors. “This is the first time that a drug with antifibrotic activity has demonstrated activity, but also very potent one, in cancer,” says Quintela, first author of the study.
The CNIO collaboration in this work started because Quintela’s group had conducted a study in 2014 in which nintedanib was applied to about 130 breast cancer patients. They then investigated whether, by adding it to chemotherapy, the drug prevented or reduced the formation of new blood vessels in the tumor.
When the group led by Mouneimne at the University of Arizona Cancer Center (Tucson, USA) was investigating the ability of nintedanib to reduce fibrosis in breast tumors, they found that Quintela’s study was the only one in the world performed on patients. At the request of his American colleagues, the CNIO again requested biopsy samples and obtained those from 73 cases, both before and after experimental treatment with nintedanib in combination with chemotherapy. After analyzing them with MeCo Score, they found that the cases with a higher fibrosis index obtained better results in terms of the benefit they could obtain from nintedanib. According to the authors, “this strategy defines a pathway toward more personalized and lower-cost treatment paradigms for breast cancer and represents the first successful clinical application targeting tumor fibrosis in oncology”.
Miguel A. Quintela specifies that this study could be “a first step towards the application for approval of the MeCo Score by the US Food and Drug Administration (FDA), although this would require information from many more clinical cases”.
Source: Spanish National Cancer Research Center
20.09.2024