© interstid – stock.adobe.com
Article • Emergency Department
Taking extra care of pregnant women with severe hypertension
Emergency care specialists must be aware of critically-important factors when treating pregnant women with severe hypertension. Experts say criteria for severely high blood pressure sits at a lower threshold for expectant mothers in comparison with non-pregnant individuals. As a result, detailed diagnosis and treatment protocols are essential with clinicians needing to adopt a specific approach when treating these patients in the Emergency Department (ED).
Report: Mark Nicholls
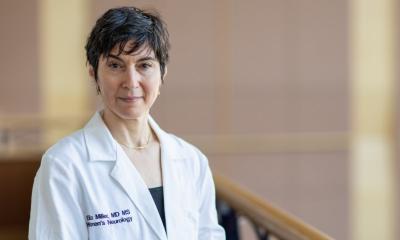
Dr Timo Suonsyrjä, Chief Physician for the Emergency Department at Helsinki University Hospital in Finland, highlighted the key approaches and warning signs during a session on Emergency Medicine in Pregnancy at the EUSEM (European Society for Emergency Medicine) 2023 conference in Barcelona. During his presentation, he said: ‘About 5-10% of pregnancies are complicated by hypertensive disorder. It is quite common, and hypertension is among the leading causes of maternal and fetal morbidity and mortality.’ However, he emphasised that it is preventable and can be treated and managed. He also underlined the importance of people being aware of their blood pressure levels.
Characteristic curves in blood pressure levels
Dr Suonsyrjä said hypertension risk factors for pregnant women include previous pregnancies, obesity, extremes of maternal age (under 18 or over 40), and pre-existing medical disease. The main hypertensive disorders of pregnancy, he explained, are chronic hypertension, gestational hypertension and preeclampsia with patient history, examination and blood, urine and uric acid tests part of the evaluation protocol. While gestational hypertension and preeclampsia are pregnancy-related, chronic hypertension is the presence of hypertension before the pregnancy; before 20 weeks of gestation; or if it continues twelve weeks after delivery. ‘Normal physiology,’ said Dr Suonsyrjä, ‘is that blood pressure levels go down during early pregnancy and then slowly up before last couple of weeks of pregnancy, so if a woman has hypertension in early pregnancy, then something is wrong.’
The threshold for severe hypertension [in pregant women] is lower compared to non-pregnant people
Timo Suonsyrjä
Patients with chronic hypertension require careful monitoring in pregnancy with their condition controlled with drugs, though with awareness that ACE inhibitors, angiotensin receptor blockers and direct renin inhibitors are contraindicated for these patients. High blood pressure in pregnant women where there are no signs of end organ complications can be treated with outpatient care with anti-hypertension medication. But it becomes an emergency care scenario needing in-patient treatment where there are signs of end organ complications and an impact on the kidneys and cardiovascular and central nervous systems.
Gestational hypertension, which normally occurs after 20 weeks of gestation, can be transient and resolved without treatment and normally after labour. ‘The most severe pregnancy-related hypertension disorder is preeclampsia or eclampsia and that needs extra follow up or even emergency care,’ the expert added.
Differences in blood pressure thresholds
In non-pregnant individuals, severely high BP is where a systolic reading is above 180 mmHG and diastolic over 110 mmHg. ‘But with pregnant women, the criteria is when the systolic reading reaches 160 mmHg, meaning that the threshold for severe hypertension is lower compared to non-pregnant people,’ said Suonsyrjä. ‘This is important because the risk of stroke is higher with pregnant women when the systolic blood pressure is over 160.’
When a severely hypertensive pregnant woman is seen in the ED, he said there is a need to establish whether it is chronic or pregnancy-related hypertension, and if there are signs of end organ damage or failure.
Blood pressure should be lowered slowly at first to avoid additional damage to vital organs and using drugs that will not have any adverse effects. Labetalol (a non-selective beta blocker), hydralazine (direct acting smooth muscle relaxant), and nifedipine (calcium channel blocker) are widely used. Suonsyrjä said treating pregnant women with severe hypertension is a multi-disciplinary team effort, including obstetric expertise, and underlined the importance of hospitals having clear protocols in this area. While there is good awareness of how to respond to such cases in the ED, he stressed the importance of acknowledging the differing threshold criteria for pregnant and non-pregnant individuals with severe hypertension.
Profile:
Dr Timo Suonsyrjä is Chief Physician in the Emergency Department of Helsinki University Hospital in Finland with a specific interest in high blood pressure and thrombosis.
05.09.2024