News • Obstetric triage
Adapted emergency care for pregnant women shows success
Increased vigilance for high blood pressure and diffuse stomach pain. These are some of the characteristics of emergency care adapted for pregnant women and new mothers.

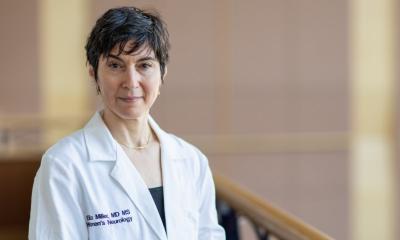
Image source: University of Gothenburg; photo: Paul Björkman
The model, which could become clinical routine throughout Sweden, is described in a thesis at the University of Gothenburg.
The aim of the thesis was to reduce morbidity and mortality among pregnant women and new mothers seeking emergency care. Sweden has relatively low rates of pregnancy-related morbidity and mortality, but pregnant women and new mothers do not currently receive the same level of emergency care as other patients.
“Despite a very low maternal mortality rate, pregnant women and new mothers can unnecessarily fall severely ill, and in a few cases even die, because the healthcare system does not identify how sick they are when they seek emergency care,” says Linnéa Lindroos, PhD student in obstetrics and gynecology at Sahlgrenska Academy at the University of Gothenburg and Senior Consultant in obstetrics at Sahlgrenska University Hospital.
The thesis describes an adapted form of what is called triage in emergency care. Triage refers to the initial and rapid assessments and prioritizations that takes place when many people seek emergency care at the same time, and it will determine how long a patient waits.
If you follow the usual triage flow, you may fail to prioritize these patients. Additionally, in case of pregnancy, we have two patients, including the baby, to consider, which makes it extra difficult
Linnéa Lindroos
The problem is that the usual triage system is not always suitable for pregnant women and new mothers. For example, elevated blood pressure in a non-pregnant patient is rarely acute in itself, blood pressure levels normally build up over time, whereas a pregnant woman with high blood pressure may be rapidly heading towards pre-eclampsia. Other conditions that require extra vigilance are bleedings that may be due to the placenta not being properly attached, or non-specific abdominal pain that may indicate premature labor. “If you follow the usual triage flow, you may fail to prioritize these patients. Additionally, in case of pregnancy, we have two patients, including the baby, to consider, which makes it extra difficult,” says Linnéa Lindroos.
She is the driving force behind the triage system, Gothenburg Obstetric Triage System (GOTS), developed, applied and evaluated in Gothenburg. The aim is not to give pregnant women and new mothers priority in the queue, but to take their physical changes and medical conditions more into account. According to the results of the thesis, the system has a good ability to reliably identify acutely ill patients. At the same time, the introduction of triage in emergency obstetric care has challenged previous approaches and procedures for this category of patients. “An important benefit is the reduction of experienced work-related stress among healthcare workers, especially midwives. The working method offers a structured approach to assessing patients, leading to more efficient decision-making and an improved overview of the patients present in the unit at the same time. Our research shows that the triage system is well accepted among midwives, nurses and doctors.”
The issue of an emergency triage system tailored to pregnant women and new mothers is particularly important in light of the increasing number of births after 40, and the fact that women are more likely to bring obesity, diabetes, high blood pressure and heart disease into pregnancy. Increased psychiatric illness in society also plays a role. “We have an ageing population giving birth, and categories of women who previously did not get pregnant. Now they can get pregnant, through better management of underlying conditions, and through IVF, but this also increases the risk of complications such as bleeding and premature birth. We rarely advise against pregnancy, but it is important that we identify deviations from the normal course of events,” concludes Linnéa Lindroos.
Source: University of Gothenburg
16.11.2023