News • Inflammatory response
Drug coat on implants reduces "foreign body" reaction
Long-term use of implantable electronic medical devices – such as pacemakers and cochlear implants – is hampered by the body’s reaction to foreign bodies. Now, in a study in mice, a team led by scientists at the University of Cambridge has shown that this reaction can be dramatically reduced by incorporating an anti-inflammatory drug into the silicone coating around the implant.
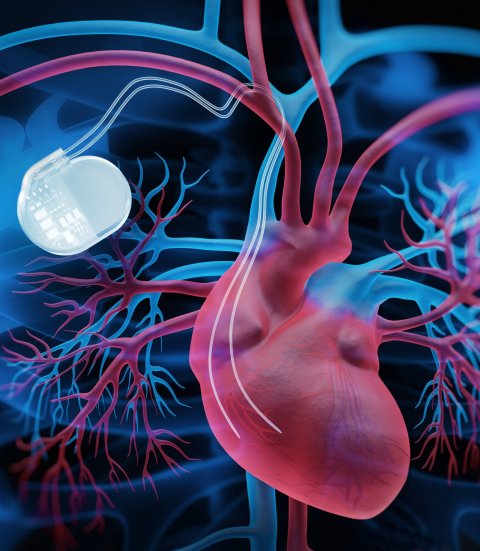
Image source: Adobe Stock/peterschreiber.media
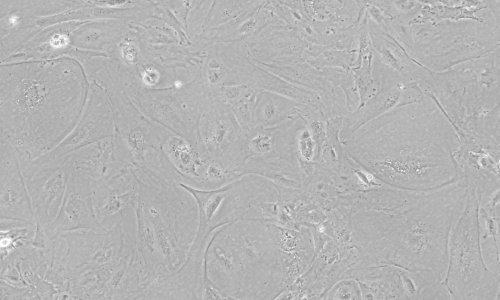
Implantable electronic medical devices are already widely used for a number of applications, but they also offer the prospect of transforming the treatment of intractable conditions, such as the use of neural electrical stimulators for spinal injury patients. There is one major problem, however: our body recognises, attacks and surrounds these implants with a dense, ‘protective’ capsule of scar tissue that prevents electrical stimulation reaching the nervous system. This so-called ‘foreign body reaction’ is driven by an inflammatory response against the implant. First, immune cells known as macrophages attack and try to destroy the device. Then a more long-term response kicks in, again coordinated by the macrophages, which leads to the build-up of a collagen-rich capsule to separate it from the surrounding tissue. This response then persists until the implant is removed from the body.
The mechanisms by which foreign body reaction occurs are poorly understood, meaning that there are no effective methods to prevent it without interfering with the tissue repair mechanisms, for example after nerve damage.
First author Dr Damiano Barone from the Department of Clinical Neurosciences at the University of Cambridge said: “Foreign body reaction is currently an unavoidable complication of implantation and is one of the leading causes of implant failure. At the moment, the only way we have of preventing it is to use broad-spectrum anti-inflammatory drugs such as dexamethasone. But these are problematic – they may stop the scarring, but they also stop the repair.”
In particular, this could make a huge difference to neuroprosthetics – prosthetics that connect to the nervous system – where the technology exists, but scarring has not yet made their widespread use viable
Clare Bryant
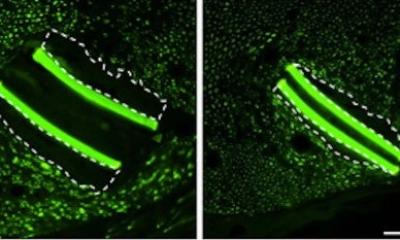
In a study published in the Proceedings of the National Academy of Sciences (PNAS), scientists implanted an electrical device into mice to compensate for sciatic nerve damage and compared the response within the surrounding tissue to that in mice who did not receive an implant. As well as using normal mice, the researchers used mice whose genes controlling the inflammatory response had been ‘knocked out’, preventing a response. This allowed the team to see how the body’s inflammatory response generated the foreign body reaction, and which genes were involved. In turn, this showed that a particular molecule known as NLRP3 plays a key role.
The researchers then added a small molecule known as MCC950 to the device coating and tested its effect in the mice. MCC950 has previously been shown to inhibit the activity of NLRP3. They found that this prevented the foreign body reaction without affecting tissue regeneration. This contrasted with dexamethasone treatment, which prevents the foreign body reaction but also blocks nerve regeneration. NLRP3 inhibitors are being developed for a number of clinical applications including inflammatory disease, cancer, sepsis, Alzheimer’s disease and Parkinson’s disease. They are already being tested in clinical trials for certain conditions.
Joint senior author Professor Clare Bryant from the Department of Medicine at the University of Cambridge said: “There’s a lot of excitement around this new class of anti-inflammatory drugs. Once they’ve been through clinical trials and have been shown to be safe to use, we should be in a good position to integrate them into the next generation of implantable devices. Combining these drugs with different materials and softer coatings for devices could transform the lives of individuals who need long-term implants to overcome serious disability or illness. In particular, this could make a huge difference to neuroprosthetics – prosthetics that connect to the nervous system – where the technology exists, but scarring has not yet made their widespread use viable.”
Source: © University of Cambridge (CC BY 4.0)
15.03.2022