Diabetes and CAD
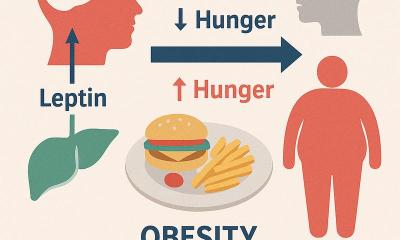
Anja Behringer reports on a neglected risk factor. With an aging population multimorbidity is increasingly a major challenge for hospital care. Diabetes is one of the medical conditions frequently encountered in multimorbid patients since cardiac and vascular diseases are often accompanied by dysfunctions of the blood sugar metabolism.

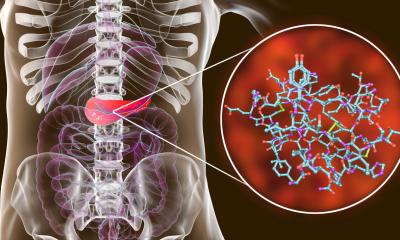
In his recent study Silent Diabetes, published last November in Diabetologica, Dresden-based cardiologist Rolf Dörr MD explored the relationship between diabetes risk and the severity of coronary artery disease (CAD). Although this relationship affects the available therapy options, many at risk patients are never identified because they are not adequately tested, Dr Dörr points out. Even more alarming, ‘different blood sugar measurement methods provide different results’. In 1,015 patients who had had a coronary angiography but who had not previously been diagnosed with diabetes, Dr Dörr and team measured HbA1c and performed an oral glucose tolerance test (oGTT), also called a blood sugar stress test. Based on the OGTT, (51% of the patients were classified with NGT (normal glucose tolerance), 1% with IFG (impaired fasting glucose), 34% with IGT (impaired glucose tolerance) and 14% were diagnosed with diabetes. According to HbA1c measurements, 58% of the patients were classified as normal, 38% as borderline and 4% were diagnosed with diabetes. These results indicate that HbA1c alone misses a substantial proportion of patients with silent diabetes and that every cardiac catheter patient with suspected or diagnosed CHD should undergo an oGTT.
The German Diabetes Foundation thus recommends oGTT and an HbA1c test to reliably identify cardiac patients at risk because in single tests too many diabetes cases remain undetected. Dr Dörr underlines that it is important to know whether patients with coronary vasoconstriction have diabetes. He explains, for example, that diabetes mellitus patients should always receive drug-coated stents to widen the arteries, while a bypass is the surgical intervention of choice when several vessels are concerned and CAD is severe.
If diabetes is properly managed then surgery, even a major intervention, is not associated with an increased risk. This, however, is not the case when complications such as CAD, neuropathy and nephropathy are present. In any case, surgery for diabetics needs special preparation and precautions by both patient and surgeon. Since stress hormones are released during surgery, the blood sugar levels increase, which means higher insulin doses are necessary. If surgery is planned for a diabetic, preparation should begin a few weeks before.
• The surgery should be discussed with a diabetologist because adequate blood glucose levels reduce post-surgery wound healing complications and infections. HbA1c should not exceed 53 mmol/mol (7%).
• The anaesthetist needs information regarding the diabetes therapy, for example whether it is drug-based (if so which medication is administered) or insulin-based. Some oral diabetes medications (sulfonylurea and Metformin) must be discontinued two days before surgery, because under surgical conditions those drugs may cause dangerous lactic acidosis.
• During 12-hour fasting before surgery the insulin dose needs to be adjusted. During surgery an infusion of 5% glucose and minerals is provided separately from the insulin via an infusion pump. During and for some time after the intervention, blood glucose is measured in 30 to 90 minute intervals and the infusion pump is adjusted accordingly. After surgery the regular insulin or medication therapy is restarted with normal meals.
* The Silent Diabetes study was co-initiated by the Forschergruppe Diabetes e.V. at Helmholtz Centre in Munich, Germany, and supported by Roche Diagnostics, a researching company and market leader in in-vitro diagnostics
18.05.2012