Demystifying pulmonary thromboembolism can change patient management
“With all that has been published in the past year on this subject, we will not lack interesting things to highlight and discuss during this session,” said Martine Remy-Jardin, MD, Head of Cardio-Thoracic Imaging at the University Centre of Lille, who will present an update on CT Imaging for thromboembolic disease on Friday afternoon at ESTI 2012.

“With CT, we have in our hands a tool that can aid tremendously in the assessment of this disease. We simply need to use it,” she said.
“I want to demystify this disease. It has a reputation to be difficult and complex,” she said. “Many radiologists will say pulmonary thromboembolism is something for an expert to interpret, which is not true; it is accessible to everyone. What requires an expertise, on the other hand, is an assessment of the thromboembolic condition to determine the correct treatment strategy.”
“For example,” she said, “emboli in the larger pulmonary arteries is a cause that should be easy for radiologists to detect.” “Peripheral thromboembolic causes are more difficult, and here,” she said, “the question becomes what the recent advances in imaging can bring to this assessment.” Central to her presentation at ESTI are the capabilities of enhanced CT technology to asses more complex patient conditions. Here clinical practice is changing. “Until recently, we had an invasive examination to assess the patient’s condition, and we can ask whether we really need this exam in pre-treatment assessment.” she said.
Even further, she suggests CT can do more. There can be a discussion in this session, on the capabilities of enhanced CT to differentiate those patents indicated for surgery and those who are not. “We have made progress in the recognition of post-surgery prognostic, but can’t we do better?” she asks. “This is a significant problem.” she said. “Surgery is such a dangerous procedure for the patient that, if possible, it should be performed only when we are confident it will work and that a patient’s condition will be improved by the surgery. There are those who will not have a prognostic that is very positive.”
“We do not have the answer to the question of whether technology changed this problem. But it is something we can begin asking at ESTI 2012,” she said, adding, “Patient management will evolve slowly, but it will change.”
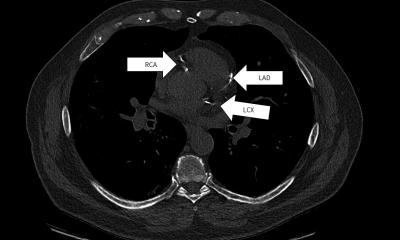
Beginning with a review of recent literature, Dr Remy-Jardin said she will demonstrate advances in imaging. “The technology now available offers us new options, allowing us to make studies that increasingly can help avoid invasive examinations,” she said. Yet pulmonary thromboembolism must be managed and treated at medical centers specialized in pulmonary hypertension. Enhancements to CT means that today a well-experienced team can avoid the aggressive angiography pulmonary examination. Images are rapidly acquired with suppression of movement in the thorax while capturing fine detail of the very small pulmonary arteries. Images of the heart are acquired at the same time, so that a reconstruction of the data set in three dimensions now offers a complete picture of the patient’s condition.
“Combining cross-sectional CT imaging with an MRI exam holds the promise of a comprehensive evaluation of the heart, circulation, and lung parenchyma with precise information that helps prevent the need for supplemental exams,” she said. “We see the trend increasing for the management of a patient,” she said. The non-invasive techniques with CT replace the need for invasive angiography, and the MRI exam replaces the need for catherization to measure hemodynamic, pressure, and resistance. “We see clearly now that that pre-therapeutic assessment of thromboembolism using the combined exams challenge the conventional first-in-line preference for catheter pulmonary angiography as well as ventilation-perfusion scintigraphy.
Dr Remy-Jardin said her presentation will also cover concerns for radiation exposure in using CT.
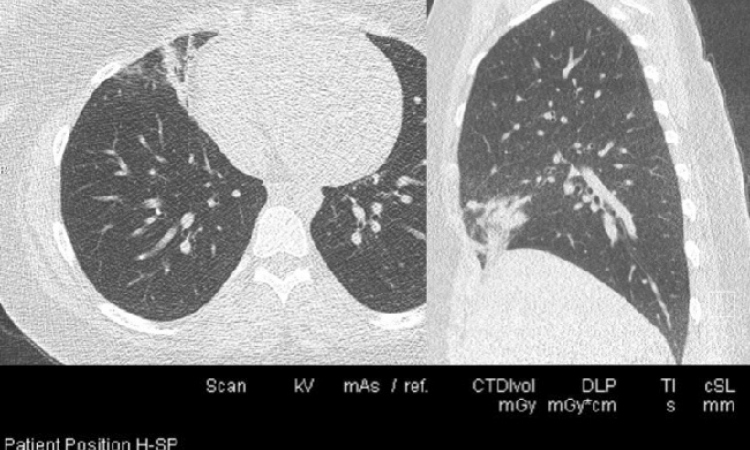
The Cardio-Thoracic Imaging group in Lille is now preparing for publication the results of its work that she said finds the diagnostic quality of images is unchanged using low-dose iterative reconstruction techniques now available. “In a first step iterative reconstruction was introduced to thoracic imaging, and we made a determination this technique can render images that are diagnostic,” she said. “In a second step, where we are now completing our work, we assess very precisely the strengths of iterative reconstruction for identifying abnormalities.”
The Lille radiology group demonstrates that quality is absolutely super imposable without any impact on the ability to distinguish the smallest anomalies. “We have been able to identify the very slight indications for infiltration in the lung, the small anomalies that are difficult to detect,” she said. “And as with other studies, we can demonstrate and confirm iterative reconstruction as a powerful tool for reducing dose without diminishing the quality and has no effect on our ability to provide a diagnosis.”
19.06.2012