Interview • Nuclear Medicine in Practice
Defining a role and routine differences
Before 2013, when Professor Dietmar Dinter became partner of Radiologie Schwetzingen, a multi-discipline group practice specialised in radiology and nuclear medicine, he was senior resident at the Institute of Clinical Radiology and Nuclear Medicine at University Hospital Mannheim (2003-2012) and head of its Nuclear Medicine Department (2009-2012). Was his work in nuclear medicine altered by the shift from hospital-based to practice-based patient care?
Interview: Sascha Keutel
Surprisingly, when asked about key differences between work in a hospital nuclear medicine department and in private practice Professor Dietmar Dinter observed that he had more time for each patient when he was a hospital radiologist. ‘In the Radiologie Schwetzingen practice there is a certain economic pressure and everything is tightly organised,’ he explained. ‘Another big difference is staff composition. While we have only fully certified specialist physicians in our practice, in a hospital teaching plays a major role – particularly in larger teaching hospitals you have many examinations in which one or two junior physicians are supervised. That takes time. ‘In a practice you gain experience more quickly due to the larger patient throughput, but you also have to arrive at the – hopefully correct – diagnostic decision more quickly.
Do the range of exams and therapies differ?
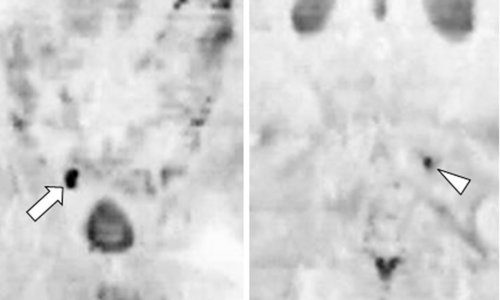
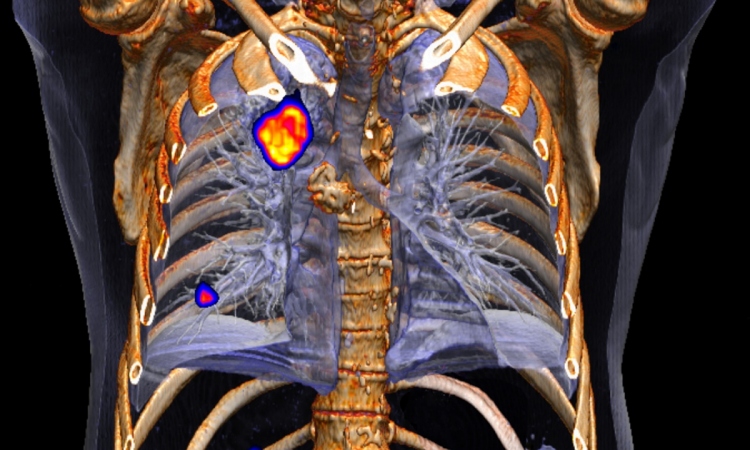
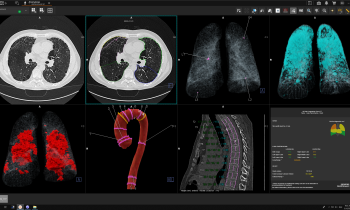
‘In Germany, radioiodine therapy is pretty much limited to hospitals, since it cannot be properly performed in private practice because German radiation protection laws require in-patient facilities – the patient has to spend at least 48 hours in a “bunker”, an entirely separate area. Most practice-based physicians do not have access to such facilities.‘There are also differences in terms of technology. Very few practices have a PET-CT, for example. That limits the range of exams compared to an emergency/out-patient facility or a hospital. Currently in Germany more than 100 PET-CT systems are installed in hospitals – most of these are operated at a loss due to the low reimbursement rates offered by statutory health insurers. ‘In some cases, hospitals cannot recover the costs of PET-CT; indeed they sometimes have to negotiate the number of exams they can perform with the health insurers. That’s impossible in private practice. The health insurers’ reimbursement parameters for PET-CT exams are clearly defined and adhered to. Lung cancer, for example, is usually imaged with PET-CT and the insurers reimburse. ‘However, the Federal Joint Committee, the relevant non-government body, decided that the costs will only reimbursed if the exam is performed in a certified lung cancer centre with the cooperation of surgeons, oncologists and radiotherapists. Thus a number of clinical specialists are needed, such as thoracic surgeons, and tumour boards must be established to discuss the case. In a practice this is close to impossible, unless you negotiate many cooperation agreements with hospitals, which then send the patients to your practice.’
Do you face many other issues that were never contemplated when working in the hospital?
'Yes, exactly: I learn a lot with all the new and different cases. The two-pronged approach in Germany with a practice-based and a hospitalbased segment creates a multitude of referral, exam and treatment paths. Most patients in practices are referred there by other office-based physicians whilst, in a hospital, you mostly see in-patients – unless the hospital has an out-patient department and thus treats in- as well as out-patients.’
Are there turf wars between hospital radiologist and those in practices?
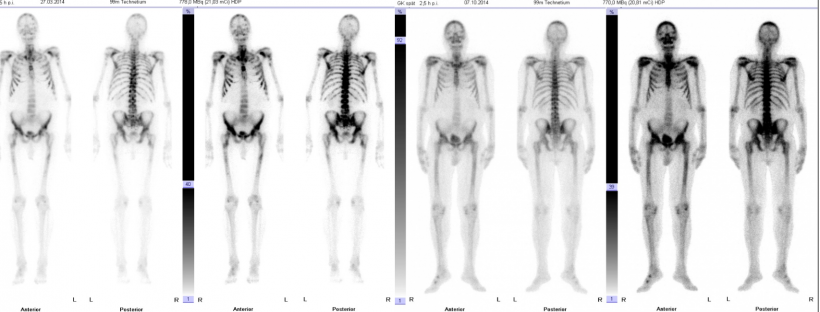
‘There are patients, particularly those who need a bone scintigraphy, who are imaged in hospital although it would be better if they were referred to a practice: practices can often offer appointments much quicker and are closer to the patients’ place of residence, so patients can be treated in a familiar environment. But there are colleagues in emergency and out-patient departments who prefer having the exams performed entirely by the in-house team.’
Do you prefer working in hospital or in a practice?

‘That’s a difficult question because there are advantages and drawbacks to both. I’d like to have more time for our patients because, as a physician, one of the main reasons to work in a practice is patient contact, particularly in diagnostic radiology. As senior resident in a hospital you often only interpret MRI or CT images without ever having seen the patient, but in a practice many exams are scheduled per physician, so you have three to six minutes to talk to a patient. This is just not enough time to communicate a diagnosis that might change the patient’s life. However, you do get used to the advantages of a practice very quickly and take them for granted: no overtime, no weekend duty, better pay.
Profile:
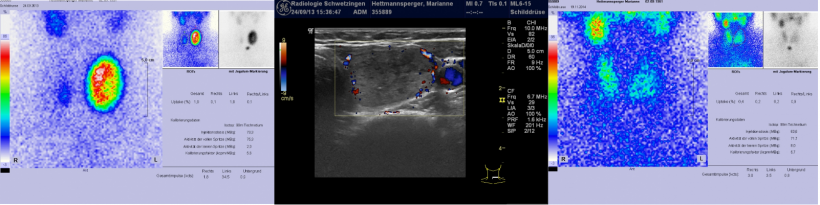
A medical graduate in 1995, Dietmar Dinter completed his radiology training in 2001 and nuclear medicine in 2009. After gaining his doctorate (1997) he focused his research on musculoskeletal and oncology imaging, with a special interest in combining morphology and functional imaging in functional MRI and PET-CT. After his habilitation (2009), in 2012 he became adjunct professor at the Institute of Clinical Radiology and Nuclear Medicine, University Hospital Mannheim, where he was also senior resident. In 2013 the professor became a partner in Radiologie Schwetzingen, a multidiscipline group practice specialising in radiology and nuclear medicine.
07.04.2015