Article • High resolution imaging
Cone beam vs. multidetector CT: Experts discuss pros and cons
Radiology practitioners have highlighted the benefits of cone beam CT in delivering high resolution at a low dose. Delegates at ECR 2023 in Vienna heard how cone beam CT (CBCT) could replace multidetector CT (MDCT) in some areas and is already showing cost-effectiveness benefits.
Report: Mark Nicholls
The aim of the session, entitled “High resolution at low dose: where and why cone-beam CT will replace multidetector CT”, aimed to offer an understanding of the technical principles, advantages and limitations of CBCT and where it outperforms MDCT. Current clinical applications were presented with a specific focus on the utility of CBCT in daily practice.
Expanding applications

Medical physicist Mika Kortesniemi, Adjunct Professor and Chief Physicist in the Department of Medical Imaging at the University of Helsinki, Finland, outlined the technical principles, dose and artefacts of CBCT, looking at advantages and disadvantages. ‘There are many applications and they are expanding in certain clinical indications,’ he said. ‘That includes dental and ear, nose and throat (ENT) radiology, and also for radiotherapy on-board imaging for verification of treatments.’
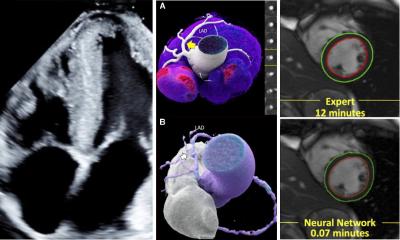
The technique is also seeing applications in interventional radiology, rotational angiography, and physical extremities in musculoskeletal (MSK) imaging, with the emerging value of the 3D beam becoming clearer. ‘CBCT can also be used in various orientations,’ Kortesniemi continued. ‘We can do weight bearing imaging for extremities, bringing added value on how the tissue structures behave under pressure of the gravitational force.’
Meaningful data and other benefits
CBCT technology is smaller and easier to install in a clinical setting with associated cost benefits as compared to MDCT, the expert pointed out. In addition, when compared to traditional 2D imaging, CBCT can offer ‘supplementary and often much more diagnostically meaningful data.’ On the other hand, he also acknowledged technical and physical shortcomings, with limited field of view and issues of heterogenous radiation dose distribution within the area that is imaged.
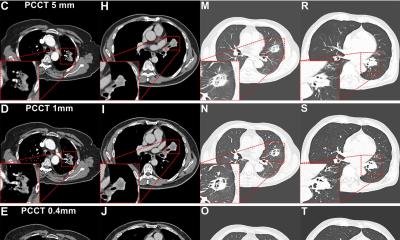
Kortesniemi highlighted the higher resolution with lower dose, pointing to Voxel sizes down to 0.1 mm and with a scalable field of view from 2-26 cm and the potential to scan the whole head, with scanners being developed capable of covering larger body regions. With the flat panel detector technology, he noted that gantry weights vary from about 60kg to more than 600kg.
One of the key optimisation strategies in CBCT is to optimise the field of view to the minimum needed for a diagnostic question. A range of different field of views have direct impact on the patient dose
Mika Kortesniemi
He said there are a limited number of projections for the raw data CBCT acquires, especially compared to multi-slice CT, which has much more projections to a rotation. The lower number of projections, in combination with limited field-of-view, means a decrease in low or soft tissue contrast and there is a longer scan time of 10-30 seconds, during which patients may move.
Most CBCT scanners use short radiation pulses rather than continually exposing patients during gantry rotation, and reconstruction time is getting shorter due to more efficient techniques, with a move towards AI-based image reconstruction. ‘One of the key optimisation strategies in CBCT is to optimise the field of view to the minimum needed for a diagnostic question,’ he said. ‘A range of different field of views have direct impact on the patient dose.’
Will technology make artifacts a thing of the past?
Artifacts – caused from metals in dental implants, for example – are an issue to consider with CBCT, Kortesniemi added. These can cause additional scatter and beam hardening. He believes that evolving image calculation and reconstruction techniques will provide better means to correct these artifacts, which may also be caused through patient movements, to improve the overall image quality.
The expert said DAP (dose area product) provides a simple and robust dosimetry unit for CBCT and avoids scatter problems in measurement. Comparing CBCT to MDCT, he said CBCT had lower performance in terms of scan time, soft tissue contrast and clinical applications, but had positives in terms of cost, required area, patient dose – to some extent – and spatial resolution.
‘The method of choice’ for head and neck region

Following up, Professor Bert De Foer, from the GZA Hospitals in Antwerp, Belgium, spoke about current clinical indications for CBCT in the head and neck, discussing its use in sinonasal, dental and temporal bone imaging. He said with CBCT, most patients are sitting upright and the X-ray source is turning around the patient and scanning on flat panel. Disadvantages of CBCT include poor soft tissue resolution, limited scan range, motion artefacts, and the process is time consuming.
However, Professor De Foer, who is also President of the European Society of Head and Neck Radiology (ESHNR) and chaired the session, added: ‘I have replaced MDCT by CBCT in the head and neck area for temporal bone, sinonasal and dental imaging since 2011 in my department and it is definitely the method of choice to do CT examinations in the head and neck region, due to its very high spatial resolution, low dose and equal quality of images in all planes.’
‘A choice for quality and lower radiation’
Sana Boudabbous from the Faculty of Medicine at the University of Geneva, Switzerland, focussed on CBCT in morphologic and functional MSK imaging. She said: ‘It gives 3D imaging with high quality, high resolution, weight bearing position is first advantage of this technique for many diseases for lower limbs and lower dose than conventional CT. The future will be reduced contrast, use of dual energy and bone quantification for example in osteoporosis.’
In closing the session, De Foer said: ‘I hope we have been successful in proving that CBCT is something completely different from MDCT and there is definitely a place for CBCT in modern radiology departments. It is a choice for quality and lower radiation.’
Profiles:
Dr Mika Kortesniemi works as the Chief Medical Physicist and Adjunct Professor at the HUS Diagnostic Center, University of Helsinki and Helsinki University Hospital, Finland. His professional, teaching and research focus is on the quality assurance, radiation dosimetry, optimisation, and radiation protection in x-ray imaging, especially related to the computed tomography and utilisation of artificial intelligence. Dr Kortesniemi is also actively involved in international collaboration with IAEA, ICRP, EFOMP and ESR.
Professor Bert De Foer is a consultant radiologist at the department of Radiology of the St Augustinus Hospital, GZA Hospitals in Antwerp, Belgium, and responsible for Head and Neck and Neuroradiology. He is president of the ESHNR and has a current scientific interest in the field of the value of MRI in the diagnosis of Menière’s disease.
16.03.2023