Image source: Adobe Stock/DragonImages
News • Prolonging life vs. maintaining functionality
Cancer treatment goals: patients and doctors often not on the same page
New research from cancer research and treatment organization City of Hope finds that only 30% of patients with advanced neuroendocrine tumors (NETs) say their top goal for treatment is living longer. The remaining patients selected other single specific treatment goals as most important, such as maintaining the ability to do daily activities, reducing or eliminating pain, or reducing or eliminating symptoms like fatigue.
66.7% of those surveyed agreed with the statement: “I would rather live a shorter life than lose my ability to take care of myself.”
The research is published in JNCCN—Journal of the National Comprehensive Cancer Network.
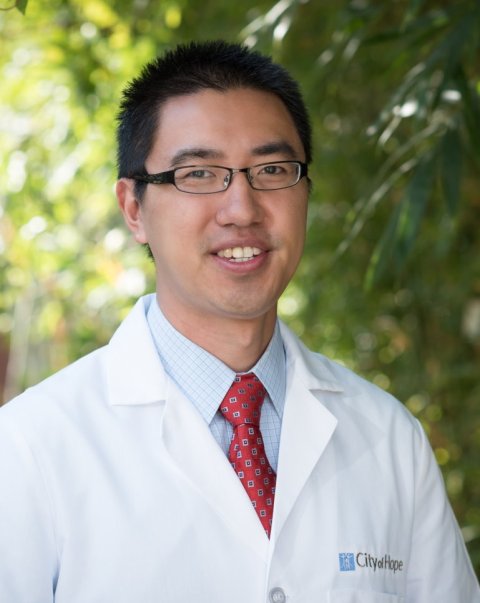
Image source: NCCN
However, respondents felt their doctors were more singularly focused on extending overall survival, even if it impacted other outcomes. Only 51.7% of patients perceived that they had the same treatment goals as their physician. “As a result of this research, I think cancer care providers need to have more honest dialogue with all of their neuroendocrine tumor patients about treatment goals and priorities of various health outcomes from treatment,” said lead researcher Daneng Li, MD, Associate Professor in the Department of Medical Oncology & Therapeutics Research at City of Hope. “This finding really challenges the traditional dogma that patients just want to live longer. Discussions regarding treatment goals are essential to ensure that health care teams are truly respecting patients’ desires for what they would like to get out of their treatment and are incorporating those preferences into the selection of overall treatment choices and planning.”
The study was conducted with 60 patients with advanced NETs of gastrointestinal, pancreatic, thoracic, or unknown primary origin, who were starting a new line of systemic therapy between March 2019 and August 2020. In order to drill down on the impact of age, half of the patients were between 18 and 64-years-old, while the other half were 65-and-older. The patients’ feelings were tracked via four different survey methods ranking the importance of various outcomes and other preference-assessment tools.
Ultimately, the decision for a specific treatment is certainly individualized, and we hope that our study sheds light on the need for better communication between care providers and patients
Daneng Li
Both younger and older patient groups ranked maintaining independence as the most valued outcome (46.7% for each), followed by survival (36.7% for younger, 23.3% for older), reducing or eliminating pain (16.7% and 6.7%), and reducing or eliminating dizziness, fatigue, and/or shortness of breath (0% and 23.3%).
“Patients with a cancer type that typically has a longer life expectancy often come to understand that the treatment journey is more of a marathon than a sprint. For these patients especially, the impact of treatment on how they feel on a day-to-day basis could impact their decision when choosing between various treatment options,” said Dr. Li. “Ultimately, the decision for a specific treatment is certainly individualized, and we hope that our study sheds light on the need for better communication between care providers and patients with neuroendocrine tumors in order to fully develop personalized treatment plans that are truly in line with the goals of each patient.”
“The study by Li, et. al. highlights the importance of considering the patient perspective when caring for patients with NETs,” agreed Emily Bergsland, MD, Professor of Medicine, UCSF Helen Diller Family Comprehensive Cancer Center, Director of the UCSF Center for Neuroendocrine Tumors, and Chair of the NCCN Guidelines® Panel for Neuroendocrine Tumors, who was not involved with this research. “Using validated surveys, the investigators found that adult patients with advanced NETs strongly value maintaining independence in daily activities over survival. Importantly, only about half of patients felt they shared the same primary treatment goal as their oncologist. The findings suggest a need for further research in this area, so we can better understand how to optimize patient-provider communication and ensure integration of patient preferences in treatment planning and medical decision-making.”
Source: National Comprehensive Cancer Network
13.12.2022