C.diff associated diarrhoea
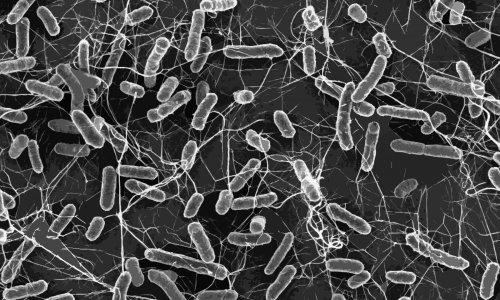
Diarrhoea caused by Clostridium difficile, which remains an issue in hospital settings, has been the focus of Cochrane Collaboration scientists, who now suggest that taking probiotics at the same time as antibiotics could help to maintain a healthy balance of bacteria in the gut, particularly as antibiotics can disturb the ecosystem of organisms normally present in the digestive system.

Although some people infected with C.diff show no symptoms, others suffer diarrhoea, colitis or, if severe, even death.
With data from 23 randomised trials involving 4,213 patients who were on antibiotic treatment for a variety of reasons examined, the review team found that 2% of patients given probiotics developed C.diff-associated diarrhoea compared with 6% of patients in the control group (typically taking placebos).
Dr Bradley Johnston, Assistant Professor at the Institute for Health Policy, Management and Evaluation at the University of Toronto and part of the Cochrane team, said: ‘Our systematic review was the first to show that some probiotics agents are both safe and effective for the primary prevention of C.diff associated diarrhoea. The pooled estimate in terms of reduced risk of C.diff associated diarrhoea was 64%.’
The researchers explored whether different probiotic species could explain the results, or whether dose was a factor. ‘We did not find any statistically significant difference based on probiotic species or dose but did find a trend to suggest that multiple species and higher dose (at least 10 billion colony forming units per day) seems to be more effective than lower dose,’ explained Dr Johnston. ‘A viable dose may be one of the most important factors when considering a probiotic agent, though there still needs to be more work on that.’
He believes implementing the appropriate dose and strains of probiotics in hospitals could provide cost savings and improve quality of life, although he accepts some clinicians may be nervous about giving live bacteria to patients, especially if they have multiple co-morbidities. ‘If patients are immune-compromised,’ he said, ‘we suggest there’s not enough evidence yet to use it in this population, but it looks like certain probiotic agents are safe in otherwise healthy adults and children.’
C.diff associated diarrhoea, especially in older adults, is a huge issue in many hospitals and nursing homes, he added, pointing to data from University of Ottawa that suggests as many as one in 10 individuals who contract C.diff die from the complications of severe diarrhoea. ‘For those who acquire C.diff, it has a major impact on patients’ quality of life; and the cost of treating such cases is substantial, with the average being around $10,000 per case,’ Dr Johnston pointed out.
The review also showed that people taking probiotics had fewer unwanted side-effects than those on placebos, including stomach cramps, nausea and taste disturbances.
The Cochrane team acknowledge that the total number of patients studied has been relatively small. However, a randomised trial (pub: The Lancet) on lactobacilli and bifido bacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE), with some 3,000 patients involved from five centres in the UK, appears to add weight to the Cochrane Collaboration findings. ‘Although the results were non-significant, when we pool the Lancet data with the previous trial data, the pooled estimate for C.diff diarrhoea suggests a risk reduction of approximately 60%, Dr Johnston said.
The baseline risk of C.diff diarrhoea is critical when considering the use of these agents, he suggested. The Lancet trial had a very low baseline risk, which might help explain why the results were non-significant. In a hospital where there is an outbreak of C.diff diarrhoea, he pointed out, prescribing certain probiotic agents at certain doses has the potential to have an immediate impact on preventing hospital acquired C.diff diarrhoea, as well as providing cost savings.
Some Canadian hospitals are already looking closely at this data and considering implementation of probiotics in outbreak settings.
Dr Johnston suggested a next step is for large head-to-head randomised trials to establish which probiotic agents work best in otherwise healthy adults. Additional work needs to be completed on the safety of probiotic agents in immune-compromised patients, and those with serious and multiple co-morbidities.
PROFILE:
Bradley Johnston MD is a scientist with Child Health Evaluative Sciences at The Hospital for Sick Children Research Institute and an assistant professor at the Institute of Health Policy, Management and Evaluation of the University of Toronto.
18.11.2013