Image source: SBI
Article • Cancer screening
The need for breast imaging for transgender patients
The need for breast cancer screening of transgender individuals has been a topic of uncertainty until recently, due to lack of reliable patient data, consensus by radiologists, published research, and recommended guidelines. A 2021 survey of Society of Breast Imaging (SBI) members revealed that ‘breast radiologists differ in their practice and knowledge regarding screening of transgender patients,’ according to the study’s principal investigator Emily B. Sonnenblick, MD, of the Icahn School of Medicine at Mount Sinai in New York City. SBI responded by sponsoring a summer webinar to discuss what radiologists need to know.
Report: Cynthia E. Keen
The Williams Institute, a Los Angeles-based research organization focused on sexual orientation and gender identity law and public policy, estimated that in 2022, over 1.6 million adults and teenagers in the United States identify as transgender, double the number it estimated in 2011. This population has a steadily increasing percentage of younger aged individuals, many believed to be undergoing gender-affirming therapy. In 2017, the Endocrine Society published guidelines endorsing the prescribing of gender-affirming hormone treatment of adolescents with gender dysphoria/gender incongruence starting at 16 years, the age of informed consent in the US.

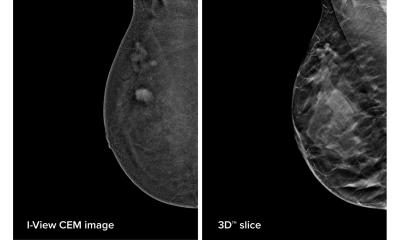
Image source: UW Health
Estrogen, which stimulates mammary development, is associated with an increased risk of breast cancer. The incidence of breast cancer in transgender individuals is unknown, due to lack of longitudinal studies and substantive data about patients. But a 2019 study from VU University Medical Centre in Amsterdam, the Netherlands, investigating the incidence and characteristics of breast cancer in 2,260 transgender women and 1,229 transgender men in the country compared with the general Dutch population revealed that transgender women had a 46-fold higher incidence of invasive breast cancer than cisgender men. Cases are rare, but they are increasingly being reported in professional medical journals.
‘Histologically, hormonal-induced breast tissue is similar to that of cisgender women,’ explained webinar presenter Mai A. Elezaby, MD, Associate Professor of Radiology at the University of Wisconsin School of Medicine and Public Health and Associate Chief of Breast Imaging at University Hospital in Madison. ‘The developing breast tissue in transfeminine patients receiving hormonal therapy is similar to cisgender women, and hence has the potential to develop the full spectrum of benign and malignant pathologies.’
Patients having “top” procedures [cosmetic breast reduction and contouring surgery] would benefit from pathologic evaluation because the breast tissue may contain significant pathology
Mai A. Elezaby
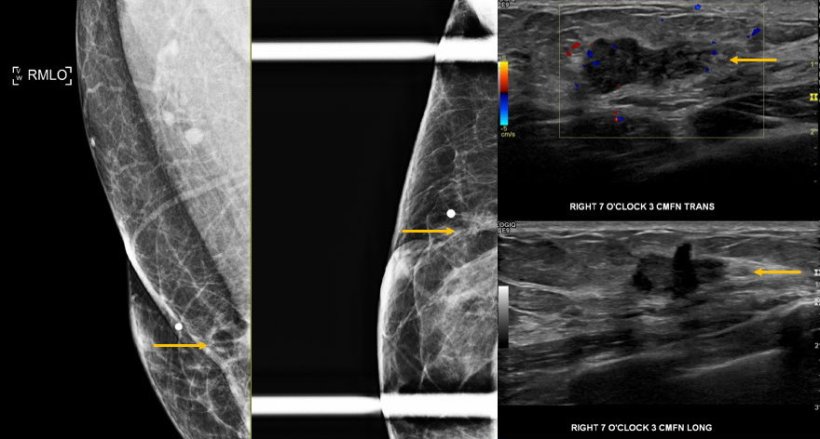
Transgender masculine patients who have breast reduction and contouring surgery rather than complete bilateral mastectomies also may be at risk because they still have some intact breast tissue. While the Dutch study showed that the 1,229 participating transgender masculine individuals had a lower rate of breast cancer than cisgender women, they still need mammography screening, especially if genetic testing identifies a BRCA mutation or they fit a moderate-to-high-risk profile. The ACR reports a lifetime risk of under 15%, 15%-20%, and over 20% for transgender men meeting average-, moderate-, and high-risk profiles respectively.
Elezaby said that it was very important for radiologists to learn what type of breast surgery transmasculine patients had undergone. Mastectomies performed for treatment of breast cancer or for risk reduction remove all breast tissue, the inframammary fold to the clavicle, and medial to lateral from the latissimus dorsi/axillary tail to the sternum. The nipple-areola complex is also likely to be removed. Although cosmetic breast reduction and contouring “top” surgery removes much of the central breast tissue, often the upper pull of the breast tissue is preserved as well as the nipple-areola complex. ‘Patients having “top” procedures would benefit from pathologic evaluation because the breast tissue may contain significant pathology. Atypia, carcinoma in situ, or invasive carcinoma can be identified in between 1.5%-4.7% of transmasculine individuals undergoing gender-affirming chest masculinization,’ she said, citing a 2020 study from pathologists at NYU Langone Health in New York City.
The ACR’s breast cancer screening guidelines, based on a person’s sex assigned at birth, risk factors, and use/duration of hormone therapy, are:
- Transfeminine individuals who have been taking hormones 5+ years should have an annual mammogram or digital breast tomosynthesis (DBT) starting at age 40 if of average risk, and between 25 and 30 years if of higher risk. Screening starting at age 25-30 should be considered for all high-risk transfeminine patients, even those not taking hormones for less than 5 years.
- Transmasculine individuals who have had reduction mammoplasty or no chest surgery should have annual mammography or DBT starting age 40 if of average risk, age 30 and older if of moderate-risk, and age 25 and older if of high-risk. A supplemental breast MRI exam may also be appropriate for high-risk individuals.
‘Radiologists need to engage healthcare providers about the importance of breast cancer screening for their transgender patients, as well as to inform patients without health insurance or who have been denied coverage of breast cancer screening exams that local, state, and national programs exist to provide financial assistance,’ urged Elezaby. ‘It’s important to take steps to create a welcoming, non-discriminatory and secure environment in radiology departments for all the diverse populations we serve.’
29.11.2022