News • Brain inflammation
AI could develop personalised psychosis therapies
A new multicentre study will investigate the link between brain inflammation and psychosis, and use artificial intelligence techniques to identify patients that might benefit most from novel treatments.
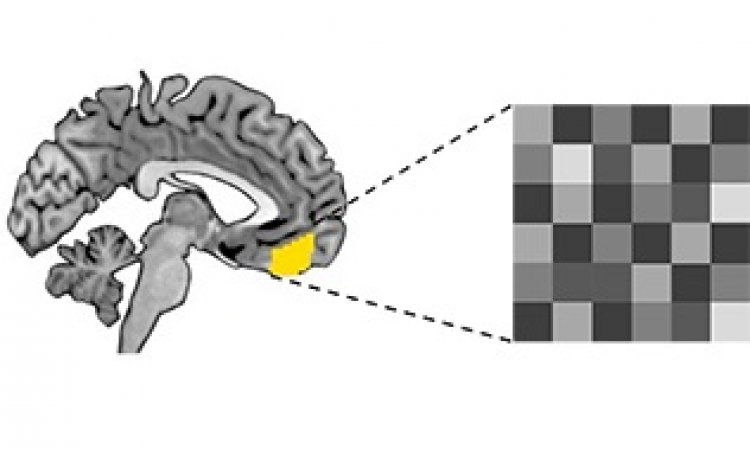
The study, funded by UKRI Medical Research Council, is led by the Universities of Birmingham and Cambridge. Researchers will examine how and if activated inflammatory cells may act differently in psychosis. For example, how they behave in circulation (blood), or whether they cross into the brain and activate immune defence cells and systems. It is possible these mechanisms could lead to psychosis, and understanding this link could open up new treatment options that target the body’s immune system.
Image source: Unsplash/Natasha Connell
Existing research has shown that some people with psychosis will also have evidence of an activated inflammatory system before and during the early stages of their condition. There is also evidence that inflammation may be related to mood symptoms such as depression, which are common in psychosis. Psychosis treatment using anti-inflammatory drugs have led to mixed results, however. This is potentially because they were given to patients with psychosis regardless of whether there was evidence of inflammation.
The PIMS (Psychosis Immune Mechanism Stratified Medicine) study will look more closely at the links between inflammation and psychosis and explore how AI techniques can help identify the patients who would benefit most from anti-inflammatory treatment. Rachel Upthegrove, Professor of Psychiatry in the University of Birmingham’s Institute for Mental Health, says: “New and more effectively targeted treatments are desperately needed for people with psychosis. Evidence suggests that inflammation may be present before and during the early stages of psychosis in some, but not all young people. Through the PIMS study, we are examining how immune dysfunction could be causally related to some symptoms of psychosis, and use Machine Learning and other AI techniques to identify who might benefit most from novel immune targeted treatments.”
Dr Golam Khandakar, in the Behavioural and Clinical Neuroscience Institute at the University of Cambridge, says: “Around one third of patients with schizophrenia do not get better with current antipsychotic medications. I am excited about working with colleagues at Birmingham and other universities involved in the PIMS project to try and understand whether in future we could target the immune system as a useful way of treating patients with schizophrenia.”
Source: University of Birmingham
20.12.2019