News • Machine learning tool
AI can predict survival of ovarian cancer patients
Researchers have created a new machine learning software that can forecast the survival rates and response to treatments of patients with ovarian cancer.
The artificial intelligence software, created by researchers at Imperial College London and the University of Melbourne, has been able to predict the prognosis of patients with ovarian cancer more accurately than current methods. It can also predict what treatment would be most effective for patients following diagnosis. The trial, published in Nature Communications took place at Hammersmith Hospital, part of Imperial College Healthcare NHS Trust. Researchers say that this new technology could help clinicians administer the best treatments to patients more quickly and paves the way for more personalised medicine. They hope that the technology can be used to stratify ovarian cancer patients into groups based on the subtle differences in the texture of their cancer on CT scans rather than classification based on what type of cancer they have, or how advanced it is.

Professor Eric Aboagye, lead author and Professor of Cancer Pharmacology and Molecular Imaging, at Imperial College London, said: “The long-term survival rates for patients with advanced ovarian cancer are poor despite the advancements made in cancer treatments. There is an urgent need to find new ways to treat the disease. Our technology is able to give clinicians more detailed and accurate information on the how patients are likely to respond to different treatments, which could enable them to make better and more targeted treatment decisions.”
Professor Andrea Rockall, co-author and Honorary Consultant Radiologist, at Imperial College Healthcare NHS Trust, added: “Artificial intelligence has the potential to transform the way healthcare is delivered and improve patient outcomes. Our software is an example of this and we hope that it can be used as a tool to help clinicians with how to best manage and treat patients with ovarian cancer.”
Ovarian cancer is the sixth most common cancer in women and usually affects women after the menopause or those with a family history of the disease. There are 6,000 new cases of ovarian cancer a year in the UK but the long-term survival rate is just 35-40 per cent as the disease is often diagnosed at a much later stage once symptoms such as bloating are noticeable. Early detection of the disease could improve survival rates. Doctors diagnose ovarian cancer in a number of ways including a blood test to look for a substance called CA125 – an indication of cancer - followed by a CT scan that uses x-rays and a computer to create detailed pictures of the ovarian tumour. This helps clinicians know how far the disease has spread and determines the type of treatment patients receive, such as surgery and chemotherapy.
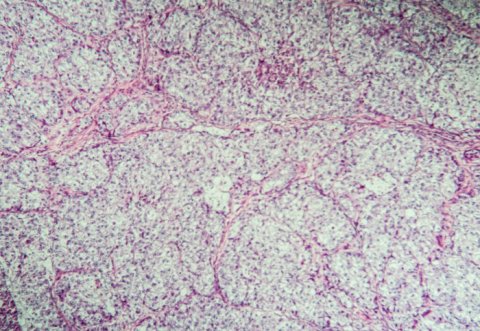
However, the scans can’t give clinicians detailed insight into patients’ likely overall outcomes or on the likely effect of a therapeutic intervention. Researchers used a mathematical software tool called TEXLab to identify the aggressiveness of tumours in CT scans and tissue samples from 364 women with ovarian cancer between 2004 and 2015. The software examined four biological characteristics of the tumours which significantly influence overall survival - structure, shape, size and genetic makeup - to assess the patients’ prognosis. The patients were then given a score known as Radiomic Prognostic Vector (RPV) which indicates how severe the disease is, ranging from mild to severe.
The researchers compared the results with blood tests and current prognostic scores used by doctors to estimate survival. They found that the software was up to four times more accurate for predicting deaths from ovarian cancer than standard methods. The team also found that five per cent of patients with high RPV scores had a survival rate of less than two years. High RPV was also associated with chemotherapy resistance and poor surgical outcomes, suggesting that RPV can be used as a potential biomarker to predict how patients would respond to treatments. Professor Aboagye suggests that this technology can be used to identify patients who are unlikely to respond to standard treatments and offer them alternative treatments. The researchers will carry out a larger study to see how accurately the software can predict the outcomes of surgery and/or drug therapies for individual patients.
Source: Imperial College London
15.02.2019