Article • Combatting nosocomial infections
A&E Staphylococci POCT
Martin Möckel and Dorothee Riedlinger, from the Charité Medical University Berlin, Emergency and Acute Medicine Campus Virchow-Klinikum, and Campus Charité-Mitte report on POCT testing in the A&E Department to screen for Staphylococcus aureus colonisation of the nose or throat.
Report: Walter Depner
People colonised with Staphylococci are at increased risk of developing a nosocomial, i.e. hospital acquired infection (HAI), the origin of which will be endogenous – i.e. the patient’s own disease reservoir. Colonisation with staphylococci is common: 20-30% of the healthy population is colonised by Methicillin-sensitive Staphylococcus aureus (MSSA), 2-3% are colonised by Methicillin-resistant Staphylococcus aureus (MRSA).

Figures on the prevalence of nosocomial infections are based on estimates. An annual 2.6 million nosocomial infections are estimated to occur within the EU, with 400,000 - 600,000 of those arising in Germany. The presence of nosocomial infections leads to extended hospital stays and treatment in intensive care, as well as to around 90,000 deaths a year across Europe.
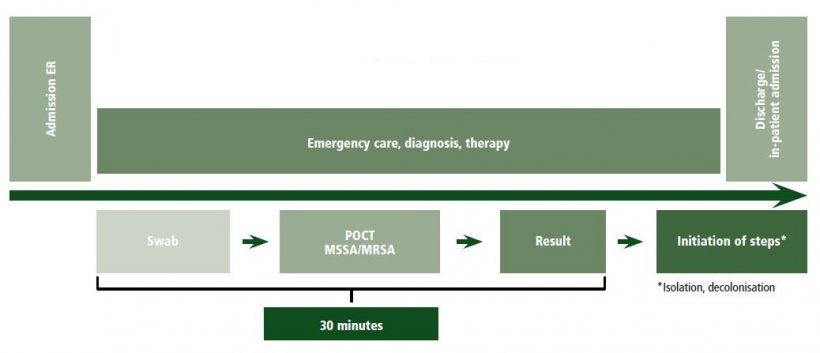
Patients suffering from acute illness are admitted to the hospital via A&E departments. The prevalence of Staphylococcus colonisation amongst those admitted via A&E is not known upon admission. However, along with acute treatment, preventive treatment, which would improve overall healthcare, can be offered in the A&E department as well. Based on this hypothesis, it was examined whether a POCT hospital admission screening system for nasopharyngeal colonisation by Staphylococcus aureus in A&E is feasible.
102 cases were examined

© Wiebke PeitzI/Charité
A&E nurses took nasopharyngeal swabs from all patients admitted to our large, inner city A&E department, irrespective of whether they were seen for out- or in-patient treatment. 102 consecutive, non-selective cases were examined using the POCT system. (The examinations were carried out using a prototype of the MSSA/MRSA-assay of the cobas LIAT system from Roche). 26.4% of these swabs tested positive for colonisation with MSSA; three swabs tested positive for MRSA. In only one case had MRSA colonisation been previously described. It was possible to integrate this screening into the A&E admission process without delay.
In the second step, nasopharyngeal swabs were taken from 1,000 consecutive patients and examined for the risk factors for MRSA colonisation, as detailed by the Robert-Koch-Institute. In this cohort, 30.4% of patients were colonised by MSSA and 2.7% were colonised by MRSA. Based on their anamnesis, only 26.1% and 59.3% respectively of those examined were at an increased risk of colonisation with MRSA, which would have called for routine screening.
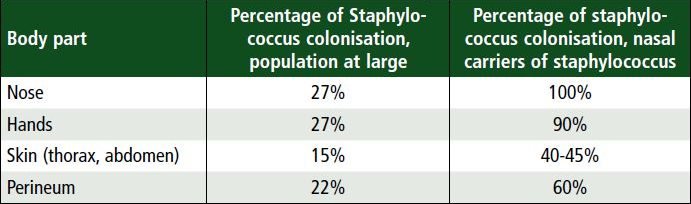
Adapted from Wertheim et al. Lancet Infect Dis 2005; 5(12):751-62
Early screening exams with fast/easy test systems
These examinations show that the cohort of those admitted to A&E have a rate of Staphylococcus colonisation similar to that described above, which indicates that early screening examinations in the context of acute care provision with fast and easy test systems is possible.
As the existing factors for risk determination only capture a part of colonised patients, it makes sense to look at other criteria for screening examinations. One option is that certain illnesses and treatments which, in turn, have a higher risk of nosocomial infections – such as invasive mechanical ventilation, emergency surgery or severe infection – should automatically involve screening and specific follow-on procedures, such as decolonisation treatment. Further analysis is required to determine which patient collectives should benefit from early screening, and studies should confirm the benefit of preventive measures, such as decolonisation treatment to reduce nosocomial infections.
The objective is to reduce the prevalence of nosocomial infections through early, specific preventive measures.
Profiles:
Martin Möckel MD is a Senior Physician, Professor of Cardiology and Head of Emergency Medicine and Acute Cardiovascular Care at Charité, University Medicine Berlin, Germany. He is also an Adjunct Professor at James Cook University, School of Public Health and Epidemiology, Townsville, Australia. The professor’s research focuses on biomarkers, healthcare in emergency and acute medicine and the implementation of interventional therapy in acute coronary care. He has led a number of multicentre trials. Martin Möckel is also part of the biomarker core groups of the Acute Cardiovascular Care Association and the 2019 congress president of the German Society for Internal Intensive Care and Emergency Medicine.
Dorothee Riedlinger is Scientific Assitant in the Emergency and Acute Medicine Campus Virchow-Klinikum, and Campus Charité-Mitte Berlin, Germany.
19.09.2019