Sponsored • Challenges in acute care
POCT: Understanding sources of error
In an emergency, point-of-care-testing can provide results in minutes. However, sources of error must be understood to ensure result accuracy and confident diagnosis (particularly important during the current pandemic).
Medical teams frequently use POCT devices to assess acutely ill patients; a hospital’s diagnostic laboratory is responsible for the analysers, plus training non-laboratory staff in their use. To explain the challenges in POCT use from different perspectives, Dr Ulf Martin Schilling (Consultant in Emergency Medicine, University Hospital of Linköping, Sweden), Dr Andrei Tintu (Clinical Chemist/Laboratory Data Officer, Erasmus University Medical Centre, Rotterdam, the Netherlands) and Professor Suzanne Bench (Professor of Critical Care Nursing, London South Bank University and the Royal National Orthopaedic Hospital, United Kingdom) spoke at a workshop sponsored by the medical technology firm BD (Becton, Dickinson and Company) during the 23rd IFCC-EFLM European Congress of Clinical Chemistry and Laboratory Medicine.

A&E (Accident and Emergency) teams often deal with acutely-ill patients where the time to diagnosis and treatment can have a direct impact on their health and outcomes. If the patient is unconscious, the clinician has no ready means of obtaining a medical history or details of relevant events that led to hospitalisation. In this situation, the doctor would typically run through a list of obvious potential causes of clinical presentation. For example, are the patient’s airways clear? Is breathing difficult? Is there a problem with circulation, as in a stroke or heart attack? Are there signs of trauma or seizure? If there are no obvious reasons for the patient’s state, a more detailed investigation is necessary. According to Dr Martin Schilling, the reasons for a patient being unconscious are generally ‘70% metabolic and 30% structural’, though the percentages vary with the patient’s age, so analysis of patients’ blood samples can help with early diagnosis and POCT typically gives results within a few minutes (a key advantage, compared to specimens tested in the laboratory).
Preanalytical variability is a key cause of poor diagnostic quality in the laboratory, shown to cause greater than 60% of all laboratory errors (Lippi G., et al. Preanalytical quality improvement: from dream to reality. Clinical Chemistry and Laboratory Medicine. 2011;49(7):1113–1126). Likewise, preanalytical variability is also critical in POCT. For example, exposure of a blood gas sample to air can result in gaseous exchange between the air and sample. This may result in the measured values of the different gases not reflecting the patient’s physiological levels. ‘Sodium,’ Schilling pointed out, ‘may be diluted if a sample is taken from the same arm in which intravenous fluids were given’ and, he reminded us, potassium levels are often elevated in haemolysed samples.
Inaccurate results can lead to misdiagnosis

In the stressful environments of an A&E and critical care units, there is the potential risk of misidentification of samples from different patients, leading to analysis of the wrong sample and resulting in the communication of erroneous values. These types of preanalytical error that cause inaccurate results can lead to misdiagnosis and, critically, potentially incorrect treatment. POCT results can help to support different potential diagnoses and may indicate which laboratory tests or imaging techniques are warranted to make a definite diagnosis and start appropriate treatment. But, according to Schilling, this is helpful only if the POCT results are accurate, as he suggests ‘we know that one in 20 results will be aberrant even by accreditation standards’.
Nurses in critical care often maintain a presence at the patient bedside, to provide physical and psychological care to the patient and support for relatives, whilst also managing complex equipment. According to Professor Suzanne Bench, this requires ‘effective communication within the wider healthcare team, supervision of junior colleagues and maintenance of accurate documentation’.
Nurses are the biggest users
Studies show that nurses value POCT because it can ‘help to speed up decision-making and delivery’ yet, Bench acknowledged, POCT can impact on nursing workload and time management. From focus group discussions with UK A&E and critical care nurses, Bench revealed that ‘nurses are the biggest users of POCT in critical care’ and nurses have a significant responsibility to clean and quality control the equipment, particularly out of hours and in smaller hospitals. Training in these operations is essential; if the equipment is not maintained properly, this can lead to inaccurate results.
Nurses report that training is necessary to ensure they understand the whole process, such as how to ensure that an accurate sample is obtained, why this is critical, and how to analyse the sample correctly. Nurses are also concerned about how POCT affects patient experience and health outcomes.
POCT blood specimen volumes are generally small (around 1 ml), but laboratory samples may be 3 ml or more. Because acutely-ill patients are monitored frequently, the volume of blood drawn may become significant, potentially leading to anaemia and, in extreme cases, requiring a blood transfusion. Preanalytical errors can exacerbate this problem, another reason why diagnostic sampling needs to be ‘right first time’.
Frequent collections from patients also cause concern about infection control and patient comfort. Bench noted that ‘the time taken for POCT also impacts on other aspects of care delivery and can lead to omissions in care provision for both the patient and the family’. For example, if the local POCT device is unavailable, a nurse may have to leave the patient and find an alternative instrument, possibly some distance away. The knock-on effect: the other nurses in the department may have to re-task to ensure coverage while their colleague is away. Therefore, having POCT systems that give reliable results are vital in critical care nursing.
Quality management

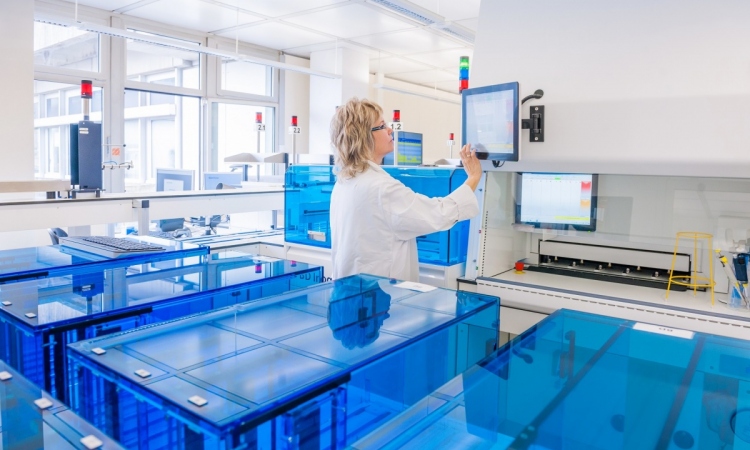
POCT devices are analytical instruments that fall within the domain of the hospital laboratory quality management, but are widely dispersed in many locations in different departments across a hospital. This creates a challenge for maintaining quality assurance and, in rare cases, the documentation of results for compliance purposes.
Generally, users of the POCT instruments are not expert in all aspects of the testing process but are medical professionals who use the instruments on an ad-hoc basis. Thus, the instruments need to be robust, fast and easy to use, and also deliver reliable results. Training clinical staff in the use of POCT instruments is a key laboratory role in many hospitals.
Dr Andrei Tintu used the example of the Erasmus University Medical Centre (4,500 POCT users) to indicate that the number of users needing training, together with the large number of POCT devices available, makes provision of the training difficult. This is an extra workload that the clinical laboratory is required to absorb. Tintu commented that, in theory, the easier a POCT instrument is to use, the simpler the training requirements should be. This may help to increase the operational efficiency and reduce costs of the clinical laboratory.
Clinical staff education
Tintu indicated that, given high staff numbers and turnover, there can be a challenge in maintaining accurate records for compliance purposes, to identify which staff are trained to use specific pieces of equipment. Educating staff on the POCT testing process and how preanalytical factors impact on sample quality, and hence the reliability of analytical results, is another vital laboratory responsibility. This helps to ensure early availability of results and fewer adverse patient events due to fewer blood re-collections.
Moreover, POCT instruments in a hospital must be verified for each sample type and test. By managing those devices, the laboratory quantifies the accuracy and reliability for the tests when conducted on these sample types, ensuring the staff obtains high quality results. The temptation for clinical users may be to test sample types which have not been verified by the laboratory’s quality management system.
The reliability and accuracy of these tests will not have been determined, increasing the risk of aberrant diagnostic results, and the eventual possibility of patient harm. To manage such use of non-validated tests, Tintu believes the best solution is robust communication between the laboratory and clinical teams. By the laboratory listening to the needs of POCT users, he believes further services could be provided to increase satisfaction among those users and ultimately improve patient care. Clearly, different groups of healthcare professionals have differing views on what POCT should provide.
What should or could POCT provide?
Blood collection devices and practices have evolved alongside the requirements of traditional diagnostic laboratory analytical instruments and, as such, are not optimised for use with POCT instruments, which are relatively new devices. Blood collection practices need to be designed and standardised to meet the different requirements of these devices. This would help to eliminate the non-standard practical methods that healthcare professionals have adopted to provide workarounds for problems found in real clinical situations.
The current COVID-19 pandemic has reminded us that safety is also critical when considering POCT, with infection control impacting on patient and staff safety. Managing acute cases increasingly depends on POCT devices maintained by healthcare science staff, operated by nurses (and others), and the results acted upon immediately by medical staff. However, despite good device maintenance and user training, sample quality and preanalytical errors can have an adverse effect on result accuracy.
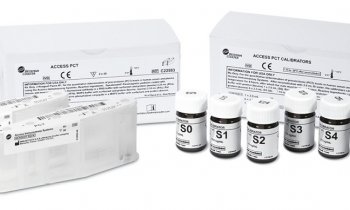
* This opinion piece is based on the authors presentations at the BD-sponsored workshop during the 23rd IFCC-EFLM European Congress of Clinical Chemistry and Laboratory Medicine. With many years’ experience in sample collection BD is investigating how to decrease preanalytical issues, to improve care of acutely-ill patients and experiences of POCT users. The new POCT BD Veritor™ System also allows for the rapid detection of influenza A and B, Group A Strep, RSV and SARS-CoV- 2 (CE approved).
15.10.2020