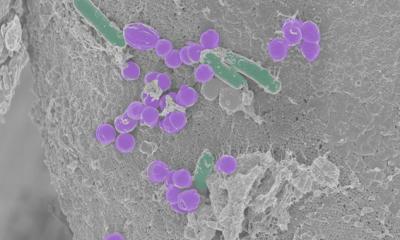
Image source: Paul Appleton, University of Dundee, via Wellcome Collection (CC BY 4.0)
News • Altered bacterial function
Accumulation of drugs in the gut may reduce their effectiveness
Common medications can accumulate in gut bacteria, a new study has found, altering bacterial function and potentially reducing the medications’ effectiveness.
These interactions - seen for many drugs including those used to treat depression, diabetes, and asthma - could help researchers to better understand how drug effectiveness and side-effects differ between individuals. The study is published in the journal Nature.
It is known that bacteria can chemically modify some drugs, a process known as biotransformation. This study, led by researchers from the Medical Research Council (MRC) Toxicology Unit at the University of Cambridge and the European Molecular Biology Laboratory (EMBL) in Germany, is the first to show that certain species of gut bacteria accumulate human drugs, altering the types of bacteria in the gut and their activity. This could change the effectiveness of the drug both directly, as the accumulation could reduce the availability of the drug to the body, and indirectly, as altered bacterial function and composition could be linked to side-effects.
The human gut naturally contains communities of hundreds of different species of bacteria, which are important in health and disease, called the gut microbiome. The composition of bacterial species varies significantly between people and has previously been shown to be associated with a wide range of conditions including obesity, immune response, and mental health.
In this study, the researchers grew 25 common gut bacteria and studied how they interacted with 15 drugs that are taken orally. The drugs were chosen to represent a range of different types of common drugs, including antidepressant medications, which are known to affect individuals dissimilarly and cause side effects such as gut problems and weight gain. The researchers tested how each of the 15 drugs interacted with the selected bacterial strains – a total of 375 bacteria-drug tests. They found 70 interactions between the bacteria and the drugs studied, of which 29 had not been previously reported.
If we can characterise how people respond depending on the composition of their microbiome, then drug treatments could be individualised
Kiran Patil
While earlier research has shown bacteria can chemically modify drugs, when the scientists studied these interactions further they found that for 17 of the 29 new interactions the drug accumulated within the bacteria without being modified. Dr Kiran Patil at the University of Cambridge’s MRC Toxicology Unit, who co-led the study, said: “It was surprising that the majority of the new interactions we saw between bacteria and drugs were the drugs accumulating in the bacteria. Until now, biotransformation was thought to be the main way that bacteria affect the availability of drugs to the body. These will likely be very personal differences between individuals, depending on the composition of their gut microbiota. We saw differences even between different strains of the same species of bacteria.”
Examples of drugs that accumulated in bacteria include antidepressant duloxetine and anti-diabetic rosiglitazone. For some drugs, such as montelukast (an asthma drug) and roflumilast (for chronic obstructive pulmonary disease), both changes happened in different bacteria - they were accumulated by some species of bacteria and modified by others. The researchers also found the bioaccumulation of drugs alters the metabolism of the accumulating bacteria. For example, the antidepressant drug duloxetine bound to several metabolic enzymes within the bacteria and altered their secreted metabolites.
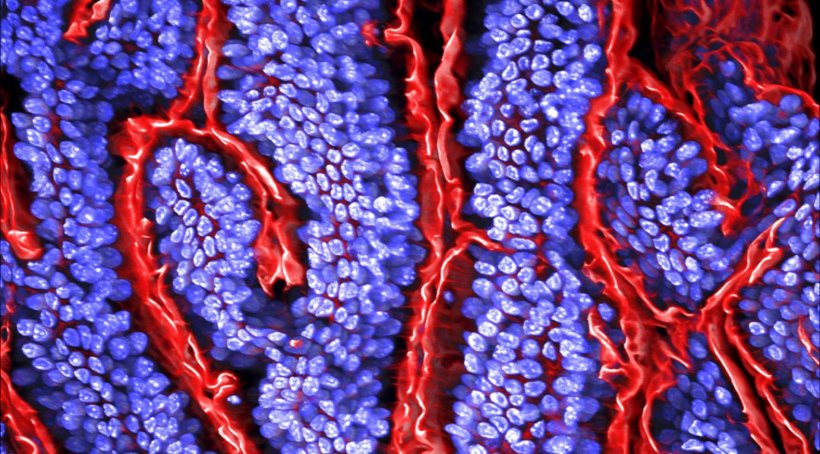
The researchers grew a small community of several bacterial species together and found the antidepressant duloxetine dramatically altered the balance of bacterial species. The drug altered the molecules produced by the drug-accumulating bacteria, which other bacteria feed on, so the consuming bacteria grew much more and unbalanced the community composition.
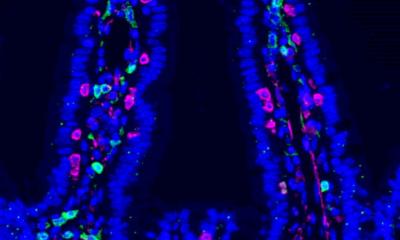
The researchers tested the effects further using C. elegans, a nematode worm commonly used to study gut bacteria. They studied duloxetine, which had been shown to accumulate in certain bacteria but not others. In worms grown with the species of bacteria that had been shown to accumulate the drug, the behavior of the worms was altered after being exposed to duloxetine, compared with worms that were grown with bacteria that did not accumulate duloxetine.
Dr Athanasios Typas at EMBL, who co-led the study, said: “Only now are people recognising that drugs and our microbiome impact each other with a critical consequence to our health.” Dr Peer Bork at EMBL, and a co-lead of the study, said: “This calls for us to start treating the microbiome as one of our organs.” Dr Patil said: “The next steps for us will be to take forward this basic molecular research and investigate how an individual’s gut bacteria tie with the differing individual responses to drugs such as antidepressants – differences in whether you respond, the drug dose needed, and side effects like weight gain. If we can characterise how people respond depending on the composition of their microbiome, then drug treatments could be individualised.”
The researchers caution that the study findings are only on bacteria grown in the lab, and more research is needed to understand how bioaccumulation of medications by gut bacteria manifests inside the human body.
Source: © University of Cambridge (CC BY 4.0)
10.09.2021