Article • Perinatology
Diagnostics and treatment of congenital heart defects
Today, many congenital heart defects can be diagnosed in the unborn child – and even treated in utero. Monique Haak (46), gynaecologist-perinatologist and fetal surgeon at Leids University Medical Center (LUMC) in Leiden, The Netherlands, is an expert in the diagnosis and surgery of fetal heart defects.
Report: Madeleine van de Wouw

But she has also become an expert in accompanying parents through an emotionally draining process. During her weekly consultation hours Dr Haak sees about eight to ten couples whose unborn child was diagnosed with a heart defect at standard anomaly scan. “In over 90 percent of these diagnoses the women affected have no risk factors; for them the diagnosis comes out of the blue. I have learned to recognize their reaction patterns: anger, disbelief, sadness. So I’ll leave them for a little while, bring them a cup of coffee and then, when the first anguish has faded, we start to talk. I do not take their emotions home, but much of my job satisfaction comes from providing comfort as much as information.”
The Netherlands lagged behind for long time
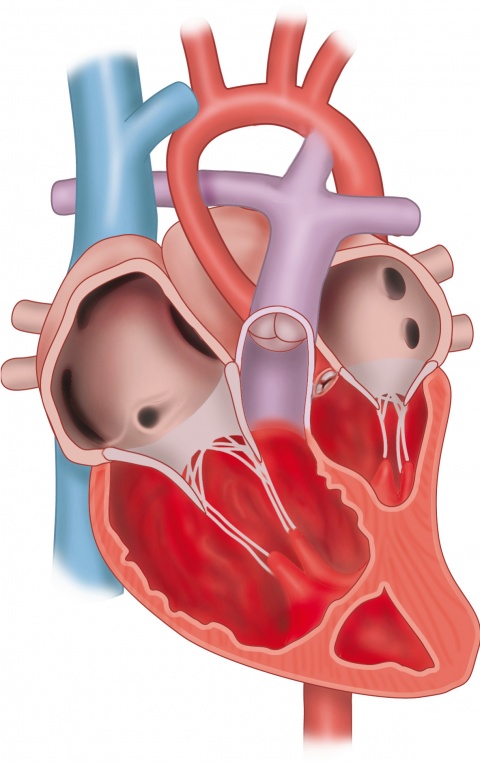
Most congenital heart defects require surgery. While some infants have to undergo surgery only once, others need multiple interventions. In any case the children remain under the control of a cardiologist for a lifetime as the effect on their health varies from minimal to life-long and severe.
Early screening and diagnosing are essential to initiate treatment as soon as possible. In many European countries, the standard anomaly scan has been a standard procedure for many years. The Netherlands lagged behind a long time, but when the standard anomaly scan was finally introduced in 2007, it made a big difference. The Dutch screening program is centrally controlled and regulated which contributes to its success. Today, around 70 percent of the severe abnormalities are detected. On European level, infrastructure and /or the size and number of rural areas need to be taken into consideration as these can influence the percentage.
Subtle changes

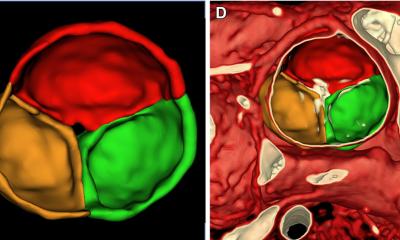
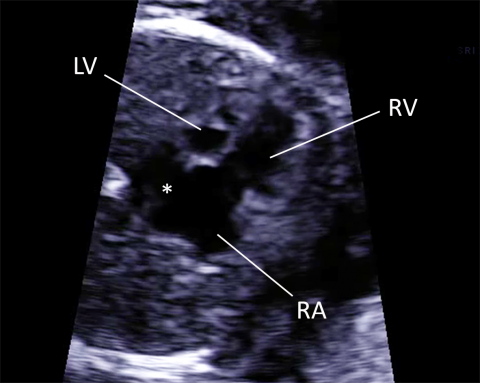
Recognizing fetal heart defects is difficult as often very subtle changes in the image are involved. The Fetal Heart Academy is a private initiative that collects an “image encyclopaedia” to show sonographers examples of heart abnormalities. “A fetal heart is very small: at twenty weeks it is the size of an adult little finger fingernail. It beats much faster than a newborn’s heart. A major abnormality is the closure of the aortic valve which may lead to poor growth and function of the left ventricle. Consequently, the blood is pumped almost completely through the right chamber. After birth, major problems arise because blood cannot be pumped to the body.”
Intrauterine interventions
An intrauterine intervention aims to open the closure of the aortic valve so the left chamber can continue to grow. A hollow needle is guided through the maternal abdomen, uterine wall and fetal chest wall into the fetal heart to open the aortic valve with an inflatable balloon. When the left chamber develops properly post intervention, life with a ‘single-chamber heart’, which involves many complications, can be prevented. For the mother, the operation, as performed in Leiden, carries no risk. The child itself is at some risk: about 5 to 10 percent die due to the surgery.
Long-term effects
Hospitals in Linz (Austria), and Toronto (Canada), pioneers in fetal heart surgery, report positive short-term outcomes but medical issues in children 5-10 years after this intervention are recently described as well. “These interventions are a clinical challenge but the question remains: Is it the right thing to do, since often the heart is already severely damaged? Strictly speaking, a long-term benefit is till unclear. For real evidence a randomized controlled trial is needed, so we would need control groups; that is children who undergo intrauterine surgery and children who undergo surgery after birth. But how would you select the women for such a trial? You can’t tell parents ‘We may be able to prevent a single-chamber heart with intra uterine surgery, but you will be randomly allocated to intra-uterine surgery or single heart surgery postnatally’ These are very difficult conversations.”
A difficult choice for parents
While timing seems to be important for the short-term result, treatment does not necessarily mean a carefree life for the child. Monique Haak invests a lot of time talking to the parents and discussing treatment options and possible consequences. “Whether they want to receive treatment, have the baby or not, these are the parents’ decision. I encourage them to follow their own heart, based on the information I gave them. Therefore we not only have clinical specialists on our team but also psychologically trained colleagues who can accompany the parents through this immensely difficult decision-making process.”
“The diagnosis of a ‘heart defect’ is a heavy burden for the parents, but at least an early diagnosis gives us and the parents time to prepare ourselves. When there is no screening, there might be an unexpected and life-threatening situation after birth. The parents take their child home, because everything looks fine in the first hours after birth. Then after a few days the baby falls ill and the child has to be rushed to a hospital and often in a poor condition. This life threatening condition, which may harm the baby's future health, can be prevented with a prenatal diagnosis. The care for the child directly after birth is adjusted to the specific diagnosis. Sometimes immediate measures have to be taken, but in some conditions the baby is comfortable with the mother during the first few hours and treatment is started later.”
“Thus, awareness raising and informing the parents are essential. At the standard anomaly scan most parents don’t realize that there might be a problem, and are only curious to know the sex of the baby. The diagnosis is a shock but after all, the proper early diagnosis of a heart defect is crucial as it can prevent brain damage by oxygen deficiency. Furthermore, both surgery outcomes and developmental outcomes are better in children with a prenatal diagnosis.”
Genetic testing
Monique Haak expects a lot of innovations in genetic testing, which is rapidly evolving. This might prove to be invaluable in the presence if a fetal heart defect. “About five percent of the unborn children that are diagnosed with a heart defect appear to have more medical problems than just that heart defect. This is very sad. Genetic testing provides insight in the risks and helps parents to make a well-informed choice. If the child has a heart defect and additional severe genetic issues, sometimes parents want to spare their child suffering and decide to end the pregnancy. Again, a choice that has to be made with full knowledge of the facts.”
Profile:
Monique Haak (46) attended Medical School at the University of Groninen, the Netherlands. Already in her third year she joined a research group on fetal physiology and learned how to perform fetal ultrasound. After Medical School she choose to work in fetal medicine and did her PhD on the early detection of fetal heart defects and the relationship of heart defects with increased Nuchal Translucency. In this project she learned how to perform basic science and to identify cardiac morphology in the laboratory of Anatomy of the Leiden University. After her PhD she trained to become a gynaecologist in the VU medical Center Amsterdam, and was staff member in that center for 6 years.
From 2011 onwards she is a fetal specialist at the department of obstetrics of the Leiden University Medical Center (LUMC). She performs fetal surgery and is specialized in the screening and diagnosis of fetal malformations. She is a known expert in fetal heart malformations and published over 100 scientific papers on ultrasound screening and improvements in diagnosis of heart defects. Because she loves teaching and believes that detection rates of heart defects can still increase she created a free-accessible image-bank: www.fetalheartacademy.org
16.09.2017