Article • Side-effects of global mobility
Multi-drug resistant bacteria: Dangerous travel companions
Trips around the globe, healthcare tourism, migration; we are mobile – and so are bacteria. Particularly dreaded are multi-drug resistant bacteria that ‘hop’ on their host during a hospital stay and are carried across the border. At MEDICA 2017 Labmed Forum Dr Andreas Ambrosch, Head of the Central Lab at Krankenhaus Barmherzige Brüder in Regensburg, Germany, will discuss these unwelcome international travel companions.

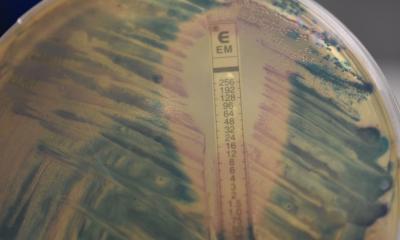
Scientists in Scandinavia, the Netherlands and Germany have conducted comprehensive research on the link between increasing human mobility and the spread of bacterial resistance. Several studies with healthy volunteer subjects showed that travellers who were initially pathogen-negative carried multidrug-resistant bacteria upon their return, in most cases ESBL-producing E. coli or Klebsiella spp. type CTX-M (ESBL = extended spectrum beta-lactamase). High-risk trips involved India (80%), followed by the rest of Asia (slightly below 50%), the Middle East and Southern Europe (approx. 15%). These and other studies found traveller’s diarrhoea and antibiotics therapies during the trip to be independent risk factors. Average length of colonisation with ESBL-producing bacteria was 30 days; in 10% of the cases, however, the pathogen continued to be present after one year. Even family members who had not travelled were infected (12%).
Healthcare tourism
According to the general, as well as the healthcare, media, in Germany infections with pan-resistant bacteria (with colistin the only therapy option left) are frequently traced back to patients who received emergency care in a foreign hospital. Thus, the first European patient to be diagnosed with carbapenemase type NDM-1 (New Delhi Metallo-beta-lactamase-1) was a Swede who had undergone treatment in New Delhi, India. Patient Zero, in a major outbreak of KPC-2 carbapenemase-producing Klebsiella at a German university hospital, had previously been treated in a Greek hospital. It took almost three years to end the outbreak: more than a hundred patients had been colonised and infected, at least 15 died of the infection. A recently published study on the incidences of multi-drug resistant bacteria in foreign hospital patients in Frankfurt reported highly resistant carbapenemase-producing bacteria, particularly Acinetobacter baumannii, in 5% of the cases. The last two patients in our facility in Regensburg found to carry Acinetobacter baumannii resp. KPC-2 Klebsiella classified as 4MDRGN (multi-drug resistant Gram-negative bacteria resistant to 4 classes of antibiotics), were previously treated in a hospital in Hungary (relating to Thailand).
Immigrant population
The high number of immigrants currently entering Germany raises public concern, politically as well as in terms of healthcare. Medically speaking, this concern is not entirely unfounded: a recent study on the prevalence of hygiene-relevant pathogens in immigrants at an admission centre in the Saarland showed 40% of the people tested to carry MDRGN resistant to two or three classes of antibiotics (for comparison: 5-10% – regional differences – among patients in German hospitals). Most frequently, E. coli or Klebsiella spp. were identified. A study testing unaccompanied minors in Frankfurt, 70% of whom hailed from Afghanistan, showed very similar results: in 34% of people tested, ESBL-producing bacteria were detected, 8% of which were categorised as 3MDRGN (incl. quinolone resistance). No pan-resistant species (4MDRGN) were found.
An updated statement by Robert Koch Institute now recommends screening of refugees upon hospital admission due to the high prevalence of multi-drug resistant bacteria in some countries of origin. However, people who underwent treatment in a foreign hospital seem to pose the greater risk, since the risk of colonisation with pan-resistant bacteria is higher in these facilities. Proactive and preventive isolation, until screening results are available, seems advisable. Travellers should be aware that, depending on their destination, colonisation with multi-drug resistant bacteria might be an unwelcome souvenir. Any physician who diagnoses such colonisation should expand the anamnesis or, if in a hospital, refer to screening. However: there is no reason to panic. Colonisation with multi-drug resistant bacteria is, in general, without symptoms. Contamination and spreading of the bacteria is most effectively prevented by adequate hand hygiene.
* The article was first published by Trillium Diagnostik 2017; 15(1):56
15.06.2017