News • Clinical cardiovascular trials
Women still underrepresented in CVD research
Women remain underrepresented in cardiovascular clinical trials despite guidelines and legal requirements developed almost 30 years ago to ensure broader inclusivity.
This is according to a report from the American College of Cardiology (ACC) Cardiovascular Disease in Women Committee published in the Journal of the American College of Cardiology. This lack of representation can limit availability of treatment data on the number one killer of women worldwide—cardiovascular disease. “Historically, drug therapies for women were determined based on male data that was extrapolated to women,” said Leslie Cho, MD, FACC, lead author of the study, a member of the ACC Cardiovascular Disease in Women Committee, and director of the Women’s Cardiovascular Center and section head of preventive cardiology and cardiac rehabilitation at Cleveland Clinic. “However, research has shown that women respond differently than men and may even be harmed or experience side effects from some drugs when taken at the same dosage as men. Sex-specific data is essential to optimal care.”
The committee issued this report to better understand the current barriers to enrollment and retention of women in clinical trials, as well as to offer novel strategies to help increase participation of women and, more specifically, underrepresented minority women, while also looking at women of childbearing age and pregnant women.
Recommended article

Article • Gender Medicine
“Inclusion of women in studies and guidelines must be increased”
Women and men are different – nobody would argue with this statement. However, in medicine, gender plays a subordinate role. Neither research, prevention nor therapy adequately reflect this difference. “This is no longer acceptable,” says internist and cardiologist Prof. Dr. Vera Regitz-Zagrosek.
The authors present eight potential barriers to optimal enrollment of women and underrepresented minority women, including:
- Differential Care – Low rates of referral to cardiologists and specialty programs for more aggressive care leads to fewer women being treated by specialists recruiting for clinical trials.
- Ageism – Older patients are disproportionately represented in clinical trials overall, which is further compounded in women as cardiovascular disease is very prevalent in older women.
- Lack of Awareness, Trust and Logistical Barriers – Previous surveys and studies have shown that women are more reluctant than men to participate in clinical trials.
- Lack of Diversity in Clinical Trial Leadership – Women are underrepresented in clinical trial leadership, and research has shown that trials led by women tend to recruit more women participants.
- Underrepresented Minority Women in Cardiovascular Clinical Trials – Clinical trials that enrolled predominantly racial/ethnic minority groups have proven that it is possible to have representation of underrepresented groups in clinical trial leadership, enrollment and retention; however, rates of minority representation in the majority of major cardiovascular trials remains low.
- Special Consideration for Pregnant Women and Women of Childbearing Age – Pregnant women and women of “child-bearing potential” are frequently excluded from clinical research as a vulnerable population, resulting in not only reduced numbers of eligible women, but a lack of data on how certain drugs impact pregnant patients.
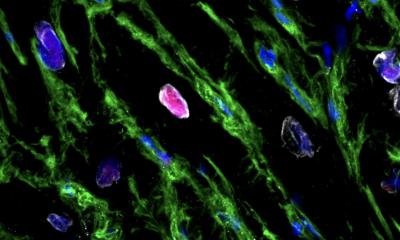
- Sex Differences in Disease – Women have a higher risk of developing certain types of heart disease and/or present with different symptoms than men when experiencing heart disease, potentially leading to lower numbers of women in clinical trials studying less prevalent types of heart disease.
- Study Retention – Little is known about potential sex differences in study drug discontinuation and patient follow up once patients are successfully enrolled since reasons for study drug discontinuation and withdrawal of consent are not routinely captured in clinical trial case reports.
Recommendations for breaking down each barrier were presented in the report, as well. “To address barriers to recruitment and retention of women in cardiovascular clinical trials, a comprehensive and targeted approach that involves partnership with all stakeholders—patients, referring clinicians, research teams (investigators and coordinators), health care systems, the FDA, payers, sponsors, professional and community organizations—is essential,” Cho said. “We owe it to our patients to increase representation of women and underrepresented minorities in cardiovascular disease trials.”
Source: American College of Cardiology
11.08.2021