Credit: IN-CSIC-UMH
News • In vivo
Magnetic resonance imaging shows brain inflammation
Research by Dr. Silvia de Santis and Dr. Santiago Canals, both from the Institute of Neurosciences UMH-CSIC (Alicante, Spain), has made it possible to visualize for the first time and in great detail brain inflammation using diffusion-weighted Magnetic Resonance Imaging. This detailed "X-ray" of inflammation cannot be obtained with conventional MRI, but requires data acquisition sequences and special mathematical models. Once the method was developed, the researchers were able to quantify the alterations in the morphology of the different cell populations involved in the inflammatory process in the brain.
An innovative strategy developed by the researchers has made possible this important breakthrough, which is published in the journal Science Advances and which may be crucial to change the course of the study and treatment of neurodegenerative diseases.
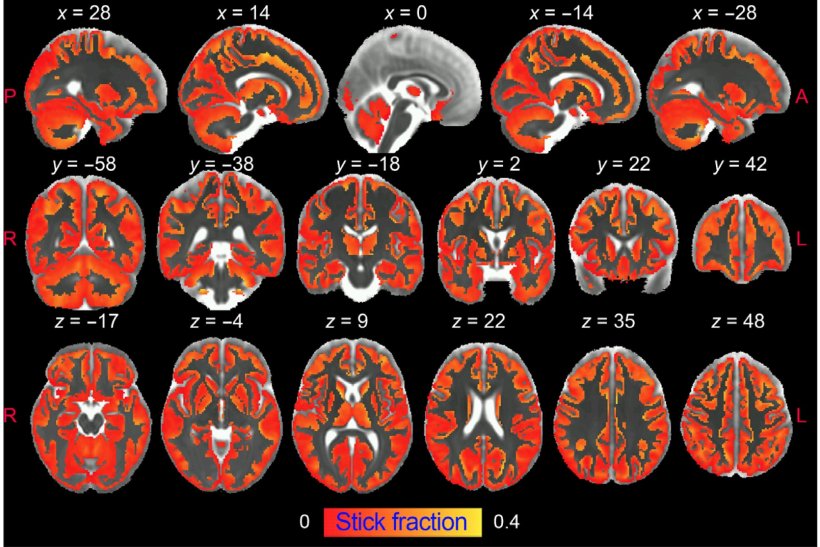
The research demonstrates that diffusion-weighted MRI can noninvasively and differentially detect the activation of microglia and astrocytes, two types of brain cells that are at the basis of neuroinflammation and its progression.
Degenerative brain diseases such as Alzheimer's and other dementias, Parkinson's or multiple sclerosis are a pressing and difficult problem to address. Sustained activation of two types of brain cells, microglia and astrocytes, leads to chronic inflammation in the brain that is one of the causes of neurodegeneration and contributes to its progression.
However, there is a lack of non-invasive approaches capable of specifically characterizing brain inflammation in vivo. The current gold standard is positron emission tomography (PET), but it is difficult to generalize and is associated with exposure to ionizing radiation, so its use is limited in vulnerable populations and in longitudinal studies, which require the use of PET repeatedly over a period of years, as is the case in neurodegenerative diseases.
Another drawback of PET is its low spatial resolution, which makes it unsuitable for imaging small structures, with the added drawback that inflammation-specific radiotracers are expressed in multiple cell types (microglia, astrocytes and endothelium), making it impossible to differentiate between them.
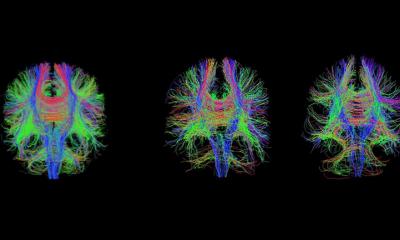
In the face of these drawbacks, diffusion-weighted MRI has the unique ability to image brain microstructure in vivo noninvasively and with high resolution by capturing the random movement of water molecules in the brain parenchyma to generate contrast in MRI images.
Innovative strategy
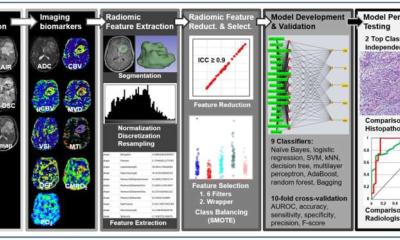
In this study, researchers from the UMH-CSIC Neurosciences Institute have developed an innovative strategy that allows imaging of microglial and astrocyte activation in the gray matter of the brain using diffusion-weighted magnetic resonance imaging (dw-MRI).
"This is the first time it has been shown that the signal from this type of MRI (dw-MRI) can detect microglial and astrocyte activation, with specific footprints for each cell population. This strategy we have used reflects the morphological changes validated post-mortem by quantitative immunohistochemistry," the researchers note.
They have also shown that this technique is sensitive and specific for detecting inflammation with and without neurodegeneration, so that both conditions can be differentiated. In addition, it makes it possible to discriminate between inflammation and demyelination characteristic of multiple sclerosis.
Silvia de Santis says this work also demonstrates the translational value of the approach used in a cohort of healthy humans at high resolution "in which we performed a reproducibility analysis. The significant association with known microglia density patterns in the human brain supports the usefulness of the method for generating reliable glia biomarkers. We believe that characterizing, using this technique, relevant aspects of tissue microstructure during inflammation, noninvasively and longitudinally, can have a tremendous impact on our understanding of the pathophysiology of many brain conditions, and can transform current diagnostic practice and treatment monitoring strategies for neurodegenerative diseases."
To validate the model, the researchers have used an established paradigm of inflammation in rats based on intracerebral administration of lipopolysaccharide (LPS). In this paradigm, neuronal viability and morphology are preserved, while inducing, first, an activation of microglia (the brain's immune system cells), and in a delayed manner, an astrocyte response. This temporal sequence of cellular events allows glial responses to be transiently dissociated from neuronal degeneration and the signature of reactive microglia investigated independently of astrogliosis.
To isolate the imprint of astrocyte activation, the researchers repeated the experiment by pretreating the animals with an inhibitor that temporarily ablates about 90% of microglia. Subsequently using an established paradigm of neuronal damage, they tested whether the model was able to unravel neuroinflammatory "footprints" with and without concomitant neurodegeneration. "This is critical to demonstrate the utility of our approach as a platform for the discovery of biomarkers of inflammatory status in neurodegenerative diseases, where both glia activation and neuronal damage are key players," they write.
Finally, the researchers used an established paradigm of demyelination, based on focal administration of lysolecithin, to demonstrate that the biomarkers developed do not reflect the tissue alterations frequently found in brain disorders.
Source: Spanish National Research Council (CSIC)
30.05.2022