Article • Spatial cognition and neurodegeneration
When the compass fails
Where are we coming from? Where are we going? Where are we right now? Our sense of spatial orientation – a complex interaction of various cells in the brain – gives us answers to these questions. In November 2018, around 70 experts in Magdeburg discussed changes in this navigation system induced by age and illness at the ‘Interdisciplinary Symposium on Spatial Cognition in Aging and Neurodegeneration’ (iSCAN).
Report: Wolfgang Behrends
Professor Thomas Wolbers, one of the organisers, spoke with us about the problems of diagnosing orientation disturbances and how the measurement of our sense of space could help in the fight against neurodegenerative illnesses such as Alzheimer’s.

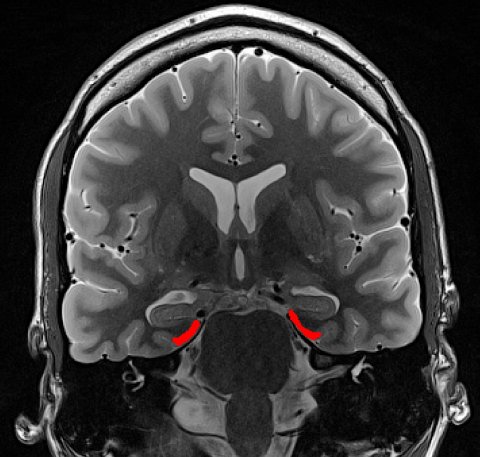
‘In our brain there are several cell types that code spatial information,’ explains Wolbers. The so-called place cells in the hippocampus and grid cells in the entorhinal cortex process the current position in the space – in principle similar to the GPS in a navigation system. Other cells function like a compass, sending signals to the head as to which direction it is oriented at any given time. This collective spatial knowledge is used by the brain to coordinate motoric impulses and thus to steer the movement of the body from A to B.
Just like a compass that no longer points North reliably after several shocks, even this orientation centre in the head can malfunction: ‘Due to brain damage in the regions where these types of cells are located, patients can develop very specific orientation disturbances.’ Using functional magnetic resonance imaging (fMRI), these disturbances can be rendered visible: Changes in the blood’s oxygen content exhibit the activity of certain brain areas in the form of voxels (spatial pixels). ‘Thus we can recognise signals transmitted by grid cells when traversing a space,’ Wolbers explained. If there is a disturbance in the sense of orientation, then these signals appear as distorted or temporally unstable. ‘That shows that the cells are no longer able to precisely compute the position in space.’
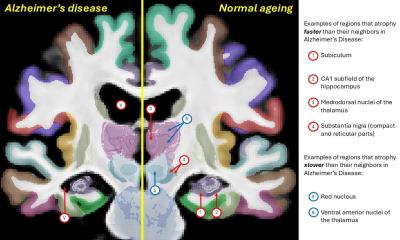
The most important disturbance factor is aging, Wolbers pointed out. ‘When we age, different neuronal deterioration processes occur in the brain. Some of the regions, like the entorhinal cortex, are particularly vulnerable to such deterioration. Thus, the spatial orientation capacity declines successively with age.’ Usually the disturbances occur first in unfamiliar environments, for example on vacation; later orientation becomes increasingly difficult even in familiar places. ‘This leads many senior citizens to adopt an avoidance attitude, so they are almost unable to move beyond their own homes. This again promotes cognitive deterioration—a vicious circle.’
Illnesses can further accelerate this disorientation. ‘The best-known example is certainly Alzheimer’s disease. Here abnormal tau proteins are deposited in the brain that can restrict the functionality of the nerve cells – and thus also cognitive performance. In some six in 10 Alzheimer’s patients this illness also has an impact on orientation – they get lost frequently, don’t find their way home without help anymore.’ Depending on which brain region is affected; even a stroke can restrict the compass in the head, just as much as psychiatric illness such as schizophrenia.
Using VR for standardised orientation tests

While the activities of the sense of orientation can be shown using fMRI, the diagnosis of the disturbances is still difficult due to a lack of standardised tests. ‘That ought to change in the coming years,’ the neuroscientist hopes. ‘There are several groups working on the development of tests by which it is possible to evaluate the seriousness of orientation disturbances.’ One of the key technologies here is virtual reality (VR): If the person being tested is given the task with 3-D visors to find his way in a virtual space, then much data is generated that can be evaluated that allows measurement of the kind and degree of disturbance. Possibly VR may even be used for therapy in cases of orientation disturbances. But there is still a long way to go before this is possible, Wolbers believes.
At the iSCAN Symposium, early recognition of cognitive deterioration processes was also strongly debated. A uniform standard to measure orientation disturbances could also serve as a significant prognosis marker. ‘Alzheimer’s has a degenerative effect’, Wolbers noted. ‘This means that the illness has already been progressing in many patients for 10 to 15 years before the first diagnosis is made. Currently, there is still no therapy. But, when a treatment is developed, it is of enormous importance that the signs of the illness are recognised as early as possible. Disturbances in the sense of orientation could be such an indicator.’
Profile:
Professor Thomas Wolbers heads a working group at the German Centre for Neurodegenerative Illnesses (Deutsches Zentrum für Neurodegenerative Erkrankungen (DZNE)) in Magdeburg and is among the organisers of the ‘Interdisciplinary Symposium on Spatial Cognition in Aging and Neurodegeneration’ (iSCAN). A specialist in age-related and illness-induced changes in cognition, his research investigates neurodegenerative processes, the development of standardised neuropsychological diagnostics and training methods to avoid neuronal deficit as well as the restoration of cognitive functions.
28.03.2019