Sponsored • Fast Ultrasound
Ultrasound system sharpens paediatric hepatic imaging
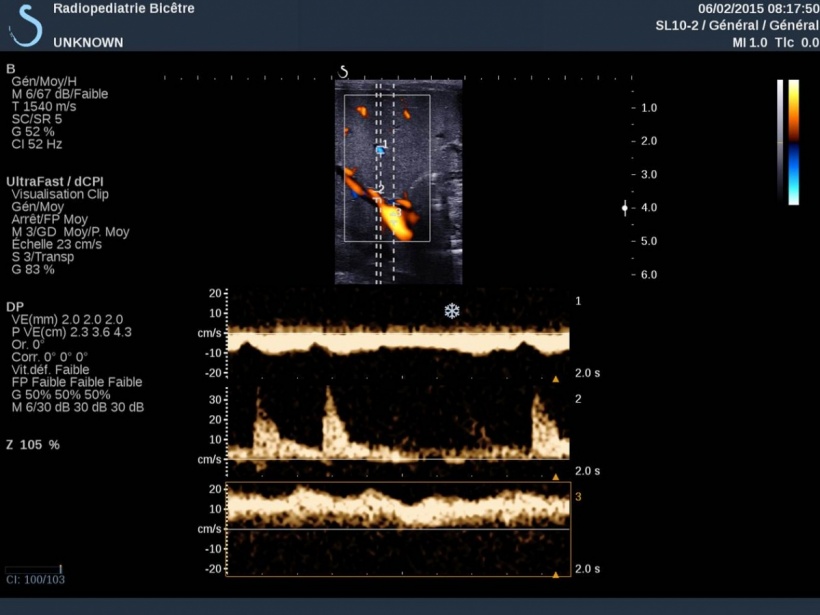
Ask about UltraFast ultrasound and you might expect a technical answer explaining why the ultrasound is faster. However, for Stéphanie Franchi-Abella MD, fast means just fast, an ultra-quick acquisition she can take of a squirming, agitated new-born in the blink of an eye. ‘These babies are small and breathing rapidly, the organs are moving fast in the image and it’s sometimes difficult to record Pulsed Wave Spectral Doppler in their vessels that are small.

‘UltraFast facilitates Doppler acquisitions. It only takes two seconds to record all Doppler data in an image and you can obtain all conventional Pulsed Wave Spectral Doppler measurements retrospectively and assess the blood flow in these vessels recorded in the image. This is interesting in young patients because one acquisition may be sufficient to assess arterial and vein patency.
‘In liver disorders it is very interesting in showing transient inversion of peripheral portal blood flow that we would not be able to see with a Doppler. For us, this can be a sign of portal hypertension,’ explained Dr Franchi-Abella, who is a paediatric radiologist at Bicêtre Hospital in Paris, the leading tertiary centre for paediatric liver disease and liver transplantation in France.
At this year’s ECR she is presenting a lecture on ‘The Benefits of Using UltraFast Ultrasound Imaging in Paediatric Patients’ during the SuperSonic Imagine Satellite Symposium.

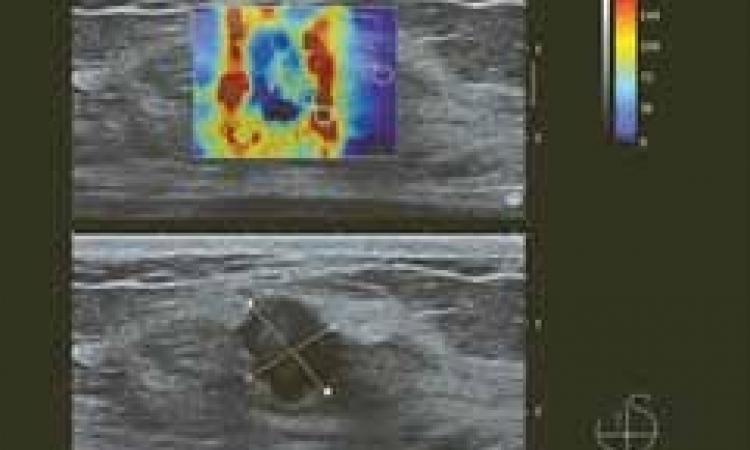
In 2012, her clinic was first equipped with an Aixplorer ultrasound platform from SuperSonic and the following year the group presented at JFR (the French meeting of Radiology and ESPR (European Congress of Paediatric Radiology) preliminary findings from a study of 98 children, half of whom were healthy while the others had liver fibrosis. The study compared the metrics reported by the ShearWave Elastography function on the Aixplorer with histological staging of biopsies from the same tissue. ‘In 90% of cases the ShearWave Elastography (SWE) matched the liver fibrosis staging obtained from biopsy,’ Dr Franchi-Abella said.
An article reporting these preliminary findings is now in press with the journal Radiology. Meanwhile these results caught the interest of the French ministry for health, which is co-sponsoring an expanded study that will enroll over 200 children to establish and validate SWE as a non-invasive tool for the diagnosis of liver fibrosis. ‘I would not want to promote any findings ahead of the definitive results; but, what is clear, and what we can say, is that the preliminary findings are very encouraging. There may be a possibility that we can better decide when to perform biopsy in certain indications,’ she said.
While the primary endpoint of establishing a correlation between histology reports and SWE remains the same, the method for analysing the histological samples calls for a computer-assisted assessment. ‘In other words, instead of having only a visual assessment, where the pathologist looks at a slide, we will scan the slide for an additional and more objective assessment with software analysis,’ Dr Franchi-Abella explained. ‘We expect to be able to complete this study next year.’
In her ECR symposium presentation, the expert said she will discuss specific applications of Aixplorer, both for its advanced UltraFast functions and elastography, as well as for its B-mode, ‘although I plan to show examples of how we apply the Ultrafast ultrasound in clinical practice, notably for liver disorders,’ she said. ‘We have had high-end ultrasound systems with complicated keyboards and so many buttons everywhere that there is nothing natural about learning how to use them. The Aixplorer has proven to be so much simpler to use that most radiologists in our service have taken it up easily and rapidly. It quickly became the preferred system for everyone in our clinic. It is the “go-to” ultrasound system because of the high-quality imaging.’
The multi-task Aixplorer can cover routine clinical assessments of morphology, whether for a neo-natal brain, or the hips, and notably for the digestive anatomy, she added. ‘We have improved our diagnostic performance in some disorders since using the Aixplorer. For example in biliary atresia – a progressive biliary fibrosis leading to biliary obstruction in new-borns – the presence of a microcyst (<0.5 mm) next to the portal bifurcation is quasi pathognomonic of this disorder. The quality of the SL10-2 probe improved the detection of such microcysts a lot, and that is helpful in assessing this pathology. For this diagnosis we don’t want to lose any time. Babies who have surgery before 40 days have a better outcome with a greater chance to resolve the pathology and avoid liver transplantation, so it is essential to make a diagnosis as early and as quickly as possible.
‘The fact that we have advanced functions for measuring liver stiffness, or to better see microvasculature, helps us to understand certain pathologies better. For children receiving liver transplants, the first month can be complicated with many things that could happen (rejection, infection, vascular disorders and so on).
‘Sometimes the ability to link a morphological image with elastometrics helps to understand what is happening better and make a much more precise diagnosis. I’ll be sharing examples from such cases of children with a liver transplant in my ECR presentation.’
06.03.2015
- congresses (700)
- liver (109)
- manufacturers (210)
- medical technology (1554)
- radiology (730)
- ultrasound (766)