Study proves benefits of ShearWave Elastography
The multinational, multicentre Breast Elastography 1 (BE1) study – launched in April 2008 and led by Professor David Cosgrove of Imperial College of Medicine, London – has shown the clinical benefits of ShearWave Elastography in ultrasonic diagnoses of breast lesions.
The study, involving 17 prestigious American and European sites -- the Imperial College of Medicine London, Hammersmith Hospital, London (UK), Curie Institute of Paris (France), DKD Wiesbaden and academic hospitals in Greifswald and Kiel, Schleswig-Holstein (Germany), Yale Medical Center and Northwestern Memorial Hospital, Chicago (USA) -- had two aims.
First, to demonstrate that images obtained using ShearWave Elastography are reproducible and then compare ultrasound alone versus ultrasound and ShearWave Elastography combined for breast lesion characterisation. The goal of the latter was to improve lesion classification in categories BI-RADS 3 and BI-RADS 4, to improve patients’ direction towards clinical short-term follow-up or biopsy.
Over 1800 breast lesions were assessed. Clinical Results:
1: ShearWave Elastography features were accurate and reproducible. To determine this, each clinical investigator was asked to perform and compare features on three separate ShearWave Elastography image acquisitions of the same lesion. Results clearly showed that ShearWave Elastography was reproducible both qualitatively and quantitatively: • Qualitative: 88% of consecutive repeated ShearWave Elastography exams were rated by physicians to be all three similar in appearance. • Quantitative*: ICC2 rates for ShearWave Elastography measurements were close to perfect, ranging from 0.84 to 0.95. Reproducibility assures a physician of a reliable and precise lesion evaluation during an exam and over time. Reproducibility is key for reporting, follow up and therapy monitoring.
2: ShearWave Elastography increased specificity and Positive Predictive Value (PPV) values.
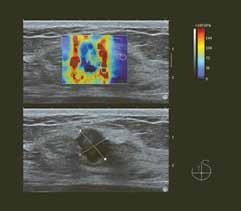
3: Using the ShearWave Elastography Maximum Value (kilopascals), ultrasound specificity increased by 26% with no loss in sensitivity and the PPV for biopsy of the BI-RADS 4a class increased by 122%. Using the ShearWave Elastography Color-Coding of Maximum Stiffness, the specificity of ultrasound diagnosis increased by 28% with no loss in sensitivity and the PPV for biopsy of the BI-RADS 4a class increased by 155%.
The outcome exceeded expectations for Claude Cohen- Bacrie, Executive Vice-President of SuperSonic Imagine and Senior Author of the two study publications. ‘The study protocol, as it was designed, did not introduce any a priori on the role of SWE as a complement to B-Mode. These published findings are providing the groundwork for a major clinical breakthrough in breast ultrasound. The results will certainly have an important impact on patient management in an area where the need for improvement in screening, diagnosis and therapy has been a driver for the entire medical community.’
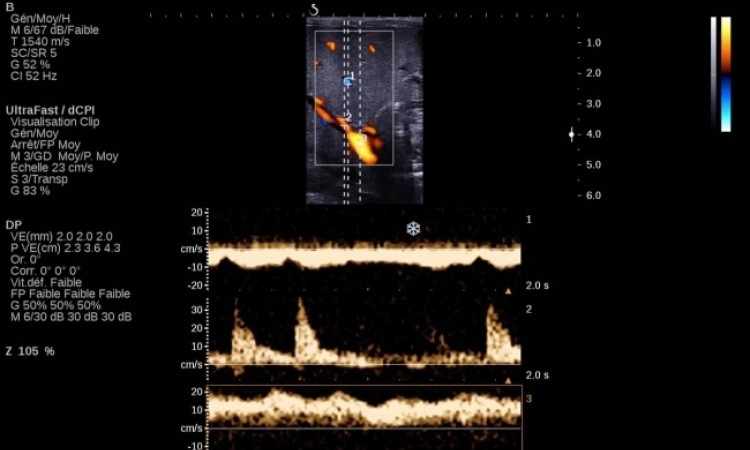
ShearWave Elastography technology provides additional, important quantitative information about tissue elasticity to ultrasound imaging. Unlike conventional elastography methods, which rely on manual compression and measure tissue displacement, no manual compression is needed and true tissue elasticity is measured by the velocity of shear waves as they propagate in tissue. Shear wave propagation speed in tissue is directly related to tissue stiffness.
The generation of a shear wave and its subsequent capture are only possible with UltraFast Imaging – acquiring images at up to 20,000 Hz, 200 times faster than conventional ultrasound. Shear wave propagation speed is calculated and the colour-coded, real-time ShearWave Elastography map produced shows quantitative (kilopascals), local tissue stiffness. ShearWave Elastography, which has been used in various organs (e.g. liver, prostate, thyroid and breast) with compelling results, is only available on the Aixplorer MultiWave Ultrasound System.
1. ShearWave Elastography for breast masses is highly reproducible. Cosgrove DO et al. European Radiology 2011 Dec
2. ICC Intraclass Correlations Coefficient
3. Shear-wave Elastography Improves the Specificity of Breast US: The BE1 Multinational Study of 939 Masses Radiology (2012 Feb;262(2):435-449) by Wendie A. Berg, MD, PhD, et al. ©
10.07.2012