True values versus relative Measurements
ShearWave elastography in prostate cancer diagnostics
Detecting prostate cancer with transrectal ultrasound using strain elastography is quite tricky: it works by applying pressure to the transducer to measure relative stiffness of tissue, Professor Correas points out and states that ‘more than 80 percent of prostate cancer develops in the peripheral zone which is against the rectal wall. If we apply pressure to this zone the deformation of the gland is not spatially homogeneous.
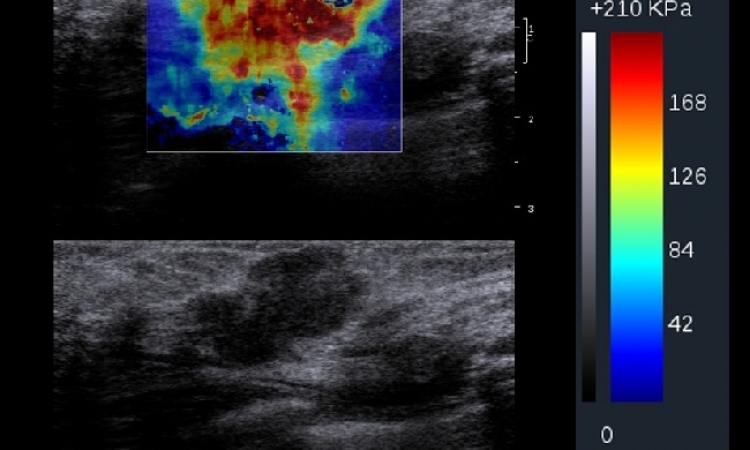
Moreover, it is difficult to apply pressure to deep areas.’ The ShearWave elastography principle is very different from strain elastography as it does not rely on manual pressure variation applied to the prostate gland. The technique does not use external pressure but leverages a unique technology that creates a shear wave and then images the shear waves as they move through tissue. In addition, Correas underlines, ‘strain elastography does not provide true tissue stiffness measurements but rather only relative measurements comparing the region of interest to the surrounding tissue. ShearWave elastography however allows accurate measurement of the shear wave velocity traveling through the tissue which in turn gives the true value of the tissue stiffness in kilopascal. We have found in our clinical practice that exceeding a elasticity measurement of 45 to 50 kilopascal results in a high probability of prostate cancer.’ Research by Professor Correas and his team has shown ShearWave Elastography to have a high sensitivity of over 80% with a high predictive positive value (over 80%), together with a high negative predictive value (90%). The new technique could be used to improve prostate cancer rate detection of transrectal ultrasonography, as well as to better target biopsies and to avoid repeating the procedure in case of negative results in patients with increasing PSA values.
ShearWave elastography is just one element in a chain of imaging modalities to detect prostate cancer but quite a relevant and reliable one. ‘Recently I had a very interesting case where MRI, B-mode and color Doppler were normal. Only ShearWave Elastography found a stiff area which was histologically confirmed as being a small cancer with significant Gleason score (revealing a rather aggressive cancer). The lesion was a small, 8 mm carcinoma, only diagnosed with this modality’, Correas explains. Due to these experiences, ShearWave Elastography is used routinely at Hôpital Necker. ‘Prostate cancer is not an easy diagnostic issue’, Correas admits. ‘ShearWave elastography could be the tool necessary to improve diagnostic confidence.’ Prof. Correas states, ‘B-mode or gray scale ultrasound imaging alone is not very sensitive with a cancer detection rate of around 40 to 50 percent. MRI is a wonderful technique and the results are highly valuable. Functional prostate MRI combines routinely T2 weighted sequences, diffusion acquisition and dynamic contrast-enhanced sequences.
However, MRI performance varies: if only a single sequence detects and characterizes a lesion as a carcinoma, the sensitivity and positive predictive values are high but the specificity is very low (below 20%); if every MR technique detects and characterizes a lesion as cancer, the specificity of the combined MR techniques slightly increases but the sensitivity drops. This is particularly true for lesions smaller than 10 mm.’ In order to improve the diagnostic rate of cancer, prostate biopsies should be targeted in the most suspicious areas.
MR prostate guidance remains too complicated, expensive and time consuming. TRUS-guided biopsy can be improved using ShearWave elastography guidance or the fusion of US data and ShearWave elastography and MRI data to take advantage of both techniques. Prof. Correas concludes, ‘a very promising future for prostate cancer detection would be three-dimensional acquisition of Shear-Wave elastography. Today, this technology is clinically used in breast exams and has great potential in the diagnostic and therapy monitoring arena. Likewise, for the prostate, 3D could assist in better detection, more accurate biopsy targeting, brachytherapy placement and follow-up of all types of treatment.`
“Aixploring the Breakthroughs Against Cancer and Fibrosis”, Supersonic Lunch Symposium, Saturday,August 27, 12:30-13:30, Hall G
Professor Jean-Michel Correas
Jean-Michel Correas is Professor of Radiology at the Paris-Descartes University and vice-chairman of the Department of Adult Radiology at Necker University Hospital, Paris, France. He received an MD PhD degree from the University of Tours and was Visiting Professor of Radiology at the University of Toronto’s Department of Imaging Research where, in the context of his Doctor of Science degree studies, he was in charge of several research projects on ultrasound contrast agents. He is deeply involved in the development of interventional uroradiology and particularly biopsy procedures and guidance as well as minimally invasive treatment of renal tumors. Prof. Correas is a member of the French Society of Radiology, the French Society of Uroradiology and the European Society of Radiology.ow-up of all types of treatment.’
25.08.2011