Image source: Konishi T et al., The Bone & Joint Journal 2024 (CC BY-NC-ND 4.0)
News • Toward better surgical outcomes
Total knee arthroplasty: a matter of alignment
When performing knee replacement surgery, also called total knee arthroplasty, doctors traditionally try to align the hip, knee, and ankle in a straight line, forming a neutral alignment, rather than replicating the patient’s original alignment.
The study was published in The Bone & Joint Journal.
When the knee is damaged due to injury or arthritis, performing daily activities like walking, sitting, and running becomes difficult due to extreme pain. In cases of severe damage, knee replacement surgery is recommended by orthopedic surgeons, to reform the damaged parts of the knee and relieve pain by attaining a neutral alignment. However, this neutral alignment is not always the patient’s original alignment and there is some debate within the orthopedic community on whether restoring the patient’s original alignment can lead to better patient-reported outcomes. In the present study, researchers have attempted to settle this debate and create a comprehensive guide on preoperative planning and execution of knee replacement surgery.
This study is mostly centered around a classification system called the Coronal Plane Alignment of the Knee (CPAK). It categorizes the possible alignments of the knee joint based on two main characteristics. First is the hip-knee-ankle angle; large negative angles cause the knees to be positioned outward, whereas large positive angles cause the knees to point inward. Meanwhile, the second characteristic is the angle of the joint line, which refers to the angle between a line level with the ground and an imaginary line going across the points where the femur meets the tibia.
This could help address the challenge of variability in patient outcomes after total knee arthroplasty by providing a more personalized approach to knee alignment, which could become a new standard in orthopedic surgery
Toshiki Konishi
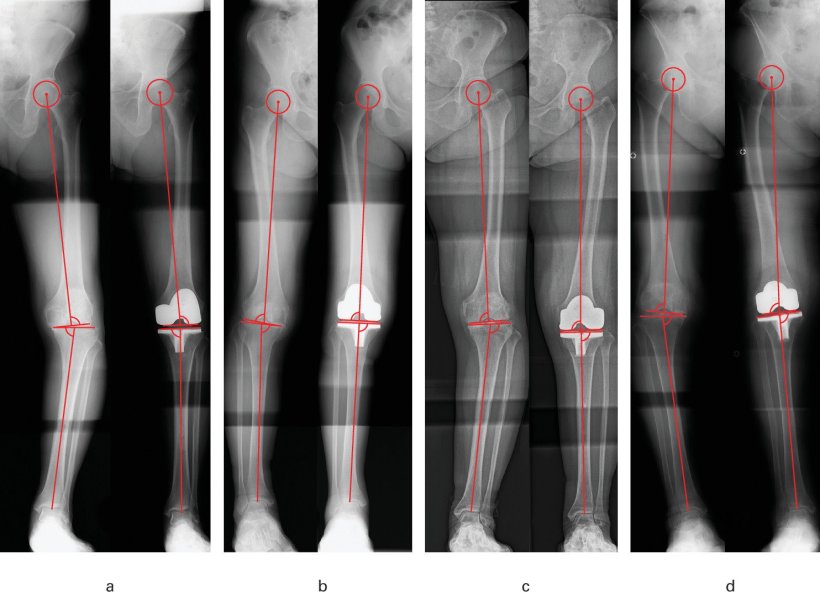
The research team, which included MD Toshiki Konishi and Associate Professor Satoshi Hamai from the Department of Orthopedic Surgery at Kyushu University Hospital, sought to determine whether changes in the CPAK categorization before and after knee replacement surgery were associated with notable differences in outcomes. To this end, they collected data from 231 patients who received knee replacement surgery for osteoarthritis at Kyushu University Hospital between 2013 and 2019. Using X-ray images, the team determined the CPAK classification and alignment variables of the patients before and after surgery. They also sent a questionnaire to the patients, from which they derived a series of standardized scores related to symptoms, overall satisfaction, activity levels, and quality of life after the operation.
After statistical analysis, the researchers revealed that patients who underwent changes in knee alignment after knee replacement surgery, as determined using the CPAK classification, had significantly worse long-term outcomes. Interestingly, they also found that patients whose joint line angle was tilted to the outside of their knee after surgery (away from the other leg) reported overall worse outcomes as well.
This study demonstrates that precisely replicating a patient’s native alignment during surgery is crucial for ensuring optimal recovery and a higher quality of life. These results could have important implications for how knee replacement surgeries are performed worldwide. “In future clinical practice, our findings may guide surgeons in preoperative planning and execution of total knee arthroplasty. By aiming to restore the patient's inherent alignment, patients can achieve superior postoperative outcomes,” explains Konishi. Adding further, he says, “This could help address the challenge of variability in patient outcomes after total knee arthroplasty by providing a more personalized approach to knee alignment, which could become a new standard in orthopedic surgery.”
Highlighting the fact that this was a retrospective study, the research team now aims to take on a prospective approach in their upcoming work. “We plan to incorporate the CPAK classification into preoperative planning, setting each patient's native knee alignment as the surgical target. Using the robot-assisted technology implemented at our institution, we are now able to perform total knee arthroplasty with high precision, ensuring the accurate reproduction of the preoperative plan,” comments Konishi.
The researchers believe that these efforts will help improve the gold standard of knee replacement surgery, leading to healthier, pain-free, and more active postoperative lives for patients.
Source: Kyushu University
06.11.2024





