Source: Pixabay/Alexas_Fotos
News • Before clinical use of antibiotics
Superbug MRSA arose in hedgehogs
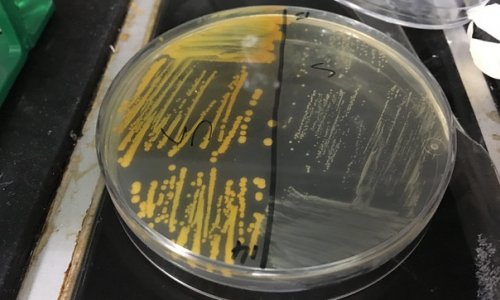
Scientists have found evidence that a type of the antibiotic resistant superbug MRSA arose in nature long before the use of antibiotics in humans and livestock, which has traditionally been blamed for its emergence.
Staphylococcus aureus first developed resistance to the antibiotic methicillin around 200 years ago, according to a large international collaboration including the University of Cambridge, the Wellcome Sanger Institute, Denmark’s Serum Statens Institut, University of Oxford and the Royal Botanic Gardens, Kew, which has traced the genetic history of the bacteria.
They were investigating the surprising discovery - from hedgehog surveys from Denmark and Sweden - that up to 60% of hedgehogs carry a type of MRSA called mecC-MRSA. The new study also found high levels of MRSA in swabs taken from hedgehogs across their range in Europe and New Zealand.
The researchers believe that antibiotic resistance evolved in Staphylococcus aureus as an adaptation to having to exist side-by-side on the skin of hedgehogs with the fungus Trichophyton erinacei, which produces its own antibiotics.
The resulting methicillin-resistant Staphylococcus aureus is better known as the superbug MRSA. The discovery of this centuries-old antibiotic resistance predates antibiotic overuse in medical and agricultural settings.
"Using sequencing technology we have traced the genes that give mecC-MRSA its antibiotic resistance all the way back to their first appearance, and found they were around in the nineteenth century," said Dr Ewan Harrison, a researcher at the Wellcome Sanger Institute and University of Cambridge and a senior author of the study.
He added: "Our study suggests that it wasn’t the use of penicillin that drove the initial emergence of MRSA, it was a natural biological process. We think MRSA evolved in a battle for survival on the skin of hedgehogs, and subsequently spread to livestock and humans through direct contact."
Recommended article

Article • Mending medication mismanagement
Antibiotic resistance: Gaining back lost ground
For many years, antibiotic consumption in France was at an alarming level, resulting in a worryingly constant increase in antibiotic resistance However, a newly-enforced strict national plan appears to be having effect.
Antibiotic resistance in bugs causing human infections was previously thought to be a modern phenomenon, driven by the clinical use of antibiotics. Misuse of antibiotics is now accelerating the process, and antibiotic resistance is rising to dangerously high levels in all parts of the world.
Since almost all the antibiotics we use today arose in nature, the researchers say it is likely that resistance to them already exists in nature too. Overuse of any antibiotic in humans or livestock will favour resistant strains of the bug, so it is only a matter of time before the antibiotic starts to lose its effectiveness.
"This study is a stark warning that when we use antibiotics, we have to use them with care. There’s a very big wildlife ‘reservoir’ where antibiotic-resistant bacteria can survive – and from there it’s a short step for them to be picked up by livestock, and then to infect humans," said Professor Mark Holmes, a researcher in the University of Cambridge’s Department of Veterinary Medicine and a senior author of the report.
In 2011, previous work led by Professor Holmes first identified mecC -MRSA in human and dairy cow populations. At the time it was assumed the strain had arisen in the cows because of the large amount of antibiotics they are routinely given.
MRSA was first identified in patients in 1960, and around 1 in 200 of all MRSA infections are caused by mecC-MRSA. Due to its resistance to antibiotics, MRSA is much harder to treat than other bacterial infections. The World Health Organization now considers MRSA one of the world’s greatest threats to human health. It is also a major challenge in livestock farming.
The findings are not a reason to fear hedgehogs, say the researchers: humans rarely get infections with mecC-MRSA, even though it has been present in hedgehogs for more than 200 years.
"It isn’t just hedgehogs that harbour antibiotic-resistant bacteria - all wildlife carries many different types of bacteria, as well as parasites, fungi and viruses," said Holmes. "Wild animals, livestock and humans are all interconnected: we all share one ecosystem. It isn’t possible to understand the evolution of antibiotic resistance unless you look at the whole system."
Hedgehog expert and co-author of the study, Dr Sophie Lund Rasmussen of WildCRU, University of Oxford explains: "Even though this finding is news to us, the hedgehogs have carried this bacterium for at least 200 years without causing any major infections in humans. Therefore, the advice is as always, to appreciate and support the hedgehogs entering your garden and to maintain a good hand hygiene when feeding and possibly handling hedgehogs. Both for the sake of the hedgehogs and ourselves."
The research was published in Nature.
Source: University of Oxford
09.01.2022