Image source: Shutterstock/Lightspring
Article • Mending medication mismanagement
Antibiotic resistance: Gaining back lost ground
France consumes more antibiotics than many other European countries – almost 30% more than average. Shockingly, outpatient prescriptions are twice the number of those in Germany or the United Kingdom, countries of comparable socio-economic standing.
Interview: Jane MacDougall
As might be expected, this high rate of usage was accompanied over time by a worryingly constant increase in antibiotic resistance; at one point, for example, Escherichia coli resistance to 3rd generation cephalosporins increased every year for 10 years. However, the strict national plan in place since the beginning of the century appears to be having effect. Since 2016, there has been a downturn in resistance in both the community and nursing homes. What is the actual situation today and how can we ensure this promising trajectory remains? We spoke with Laurent Dortet, Co-Director of the National Reference Centre for antibiotic resistance.
‘Antibiotic resistance is still a problem in France, but no more than in other countries. Many of our immediate neighbours have a greater problem than France, for example Italy or Greece. Antibiotic resistance is a worldwide problem. The WHO has identified the most problematic bacteria, essentially Gram-negative organisms, the Enterobacterales, Escherichia coli and Klebsiella spp., where resistance is caused by strains producing broad spectrum antibiotic degrading enzymes, such as carbapenamases. Also amongst the Gram-negatives there is carbapenem-resistant Pseudomonas aeruginosa. These bacteria are a particular problem because the Enterobacterales cause the majority of nosocomial infections.
‘On the other hand, while Staphylococcus aureus remains a significant pathogen, in France we have made major progress against MRSA over the past 20 years, from 30% to 15% methicillin resistance. That means we have halved our rate of MRSA. Another reason we are less bothered by the Staphylococci is because new molecules have become available giving us new therapeutic options. But for Gram-negatives our choices are much more limited. The pipeline is empty, very few molecules have come out and they are not the panacea, we don’t have a miracle cure yet.’
Factors that cause antibiotic resistance
‘A good antibiotic will lead to resistance because bacteria are fighting for survival. Resistance arises from a combination of factors. The most important is the overuse and/or misuse of antibiotics on a global, not individual level. Everything done in veterinary medicine and animal husbandry will have a knock-on effect on humans. Using antibiotics to fatten animals, pigs, chickens etc. shouldn’t be done, we need antibiotics for health. The use of antibiotics outside the hospital, aquaculture and agriculture releases large quantities of antibiotics into the environment where they can start to build up reservoirs of resistance. This needs to be reduced.’
Recommended article

News • Epidemiology & economics
Bacterial resistance costs French hospitals up to 290 million Euros per year
A team of researchers from Versailles Saint-Quentin-en-Yvelines University (UVSQ), Inserm and Pasteur Institute has been able to provide for the first time an accurate estimate of both the incidence (annual number of new cases) and added direct cost of infections due to antibiotic-resistant bacteria in patients hospitalised in French hospitals during 2015 and 2016.
French strategies that work
‘The Mission Spares which monitors resistance gives an overall vision of the situation. It allows us to compare ourselves with other countries to see what we are doing well or less well and, above all, to see the evolution. I think it’s extremely important to follow the epidemiology of resistance, regularly. We have multiplied by ten the number of species studied by the previous mission, which I think gives a more realistic idea of the situation than we had five or six years ago.
Decisions on antibiotics have to be coordinated and made on an International level, because if France does something and Belgium or Italy, for example, do nothing we’ll never solve the problem
Laurent Dortet
‘However, there is always a question mark over how we diffuse this information to the infectious disease specialists, to the doctors in the community to have action. This is always the difficult part, to translate data into practice. This is complicated by the fact that while we scientists gather the information, its dissemination is political. We can give our advice, for example we can say that a mechanism of resistance is emerging, but it’s out of our hands.
‘Decisions on antibiotics have to be coordinated and made on an International level, because if France does something and Belgium or Italy, for example, do nothing we’ll never solve the problem. Hypothetically, we can’t say in animal husbandry that we’ll reduce the use of antibiotics everywhere, then China says it want to continue to use colistin to fatten its chickens. Very quickly they’ll have resistant bacteria that will arrive here even faster than Covid-19 did.’
French antibiotic resistance
‘Hospital doctors are highly aware, especially those in large public (CHU) hospitals. I think the level of awareness is lower among general practice doctors… we are seeing less antibiotic resistance in the community. In terms of the general public, I think they are not aware at all.’
Can we raise awareness?
‘There are, and have been, many campaigns run by social security to raise awareness amongst HCPs in hospitals and the community, for example for paediatricians, to limit antibiotic prescriptions for otitis. We see this worked because the amount of resistant Pneumococus, the bacteria causing these ear infections, has reduced over the time since the campaign aired and awareness rose. Doctors now ask “Do I need to use an antibiotic for this patient, this time?” Likewise patients need to learn not expect a prescription every time, which is quite ingrained in the French. In other European countries, such as Denmark, it’s the opposite. The “antibiotics are not automatic” campaign in 2018 worked really well, but this type of campaign needs to be regular but, too many public health messages cannot be given at once and, for now, there are other priorities.’
Possible solutions
‘One thing is to offer incentives to develop new antibiotics. Developing an antibiotic costs the same as any other medicine, but the return on investment is much lower; an antibiotic is taken perhaps for a week, once in a patient’s lifetime; a statin is used every day for a patient’s lifetime. This is one reason we have no new molecules. If we want pharmaceutical companies to invest, we need to be inventive in ways to keep the process financially interesting, perhaps by extending patents for 30 or 40 years. We also need to screen rapidly, to detect where resistance is occurring. This is part of my work, developing rapid diagnostic kits to detect resistance, so we can start appropriate antibiotic therapy fast, to prevent resistance having a chance and gain back the ground we’ve lost to bacteria.’
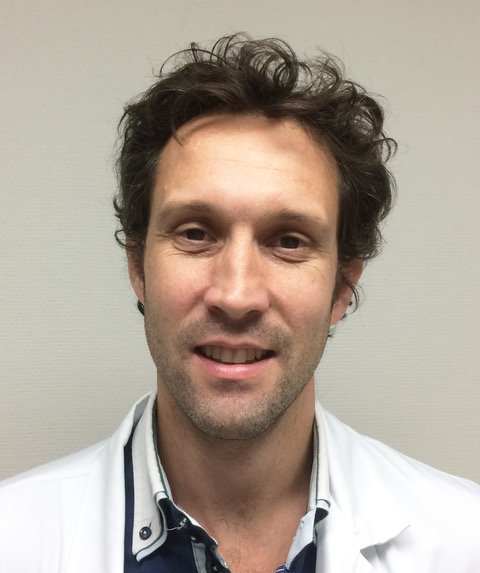
Profile:
Pharmacist Professor Laurent Dortet is Co-director of the Associated National Reference Centre for Antimicrobial Resistance and bacteriologist in the Bacteriology and Hygiene Department at the Kremlin-Bicêtre University Hospital, South of Paris. He completed his PhD in microbiology, then became a post-doctoral researcher at Imperial College, London, UK funded by a Marie Sklodowska-Curie Individual Fellowship, before returning fulltime to his role at the Kremlin-Bicêtre University Hospital.
06.01.2022