
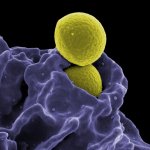
Image source: Adobe Stock/Milos
News • Reduction of healthcare-associated infections
Study: Anti-Covid measures also prevent HAIs
A new study conducted by researchers at The University of Texas MD Anderson Cancer Center suggests that enhanced infection prevention and control (IPC) measures implemented to address the Covid-19 pandemic contributed to a significant decrease in many healthcare-associated infections (HAIs) and a reduction in respiratory viral infections (RVIs).
The findings, published in the American Journal of Infection Control (AJIC), provide some of the first evidence that strict pandemic-related IPC interventions reduced HAI rates among vulnerable patient populations. “Previous, large-scale studies revealed an alarming increase in some HAIs during the pandemic, which may be partly attributed to the necessary, dramatic shift in institutional IPC priorities,” said Roy F. Chemaly, MD, MPH, Chair of Infectious Diseases, Infection Control, and Employee Health at MD Anderson, and the lead author on the published study. “Our findings suggest that enhanced and targeted IPC measures enabled our facility to avoid these increases and, in several cases, significantly reduce the incidence of HAIs among our patient population during the pandemic.”
The encouraging findings from this study suggest that prioritizing and investing in evidence-based IPC practices can reduce HAIs, even among particularly vulnerable populations during extreme situations
Patricia Jackson
Beginning in March 2020, MD Anderson deployed enhanced IPC practices to reduce the spread of Sars-CoV-2, including high-level personal protective equipment, universal masking, enhanced environmental disinfection, and visitor restrictions, among others.
Dr. Chemaly and colleagues calculated the incidence rates (IRs) of six HAIs among the approximately 30,000 patients admitted annually at the cancer center from September 2016 through March 2022: Clostridioides difficile infection (C. diff), multidrug-resistant organisms (MDROs), respiratory viral infections (RVIs) and three device-related infections — catheter-associated urinary tract infections (CAUTI), central line-associated bloodstream infections (CLABSI), and ventilator-associated events (VAE). The researchers then compared IRs for all HAIs for the 42 months prior to the pandemic (September 2016-February 2020) and the 25 months after the pandemic onset (March 2020-March 2022), as well as during the time of Covid-19 surges and in Covid-19-designated wards at the 767-bed facility.
Recommended article
Article • Microbiology & hygiene
HAIs are one problem – MDROs another
In view of the increase of multidrug-resistant organisms (MDRO), the WHO has declared antibiotic resistance one of the biggest threats to global health. MDROs have become a major problem particularly in hospitals. Professor Dr Georg Häcker from the Institute for Microbiology and Hygiene at the University Hospital Freiburg, explains some strategies to prevent hospital-acquired infections (HAIs).
Results show that the incidences of laboratory-identified C. diff (Li-CDI), CLABSI, and total RVIs at MD Anderson decreased significantly since the start of the Covid-19 pandemic. Rates of MDROs were unchanged except among patients on Covid-19 wards, and rates of other device-related infections remained stable. Specifically:
- The incidence of Li-CDI significantly decreased after the onset of the pandemic, from 6.58 cases per 10,000 patient days to 4.31, with a statistically significant incidence rate ratio (IRR) of 0.65. The Li-CDI rates were similar between surge and non-surge periods (0.43 during surge vs. 0.44 during non-surge periods).
- The total IR of nosocomial RVIs significantly decreased from the pre-pandemic to the pandemic period, from 5.24 to 1.90 per 1,000 admissions, with an IRR of 0.36. The IR did not change significantly between surge and non-surge periods. When evaluated individually, the IRs of Sars-CoV-2 and nosocomial respiratory syncytial virus (RSV) infections were significantly higher during the surge period, while the IR of nosocomial influenza infection was comparatively lower.
- The overall IRs of nosocomial MDROs were similar from the pre-pandemic to the pandemic period (0.66-0.74 with an IRR of 1.22) and did not significantly change between surge and non-surge periods (0.16 vs. 0.14). Notably, the overall IR of MDROs in the Covid-19 wards was more than five times higher than in the other inpatient wards (1.99 vs. 0.35 with an IRR of 5.77).
- The rate of CLABSI significantly decreased during the pandemic, from 0.51 to 0.32 per 1,000 catheter days (IRR of 0.63). Notably, MD Anderson recorded 100% CLABSI bundle compliance in September 2022, with central line placement and maintenance completed exclusively by trained and experienced staff.
- The rates of CAUTI (0.75-0.66; IRR of 0.88) and VAE (3.10-1.82; IRR 0.60) did not significantly change between the pre-pandemic and pandemic periods.
“The encouraging findings from this study suggest that prioritizing and investing in evidence-based IPC practices can reduce HAIs, even among particularly vulnerable populations during extreme situations such as the Covid-19 pandemic,” said Patricia Jackson, RN, BSN, MA, CIC, FAPIC, 2023 APIC president.
Source: Association for Professionals in Infection Control and Epidemiology
08.10.2023





