Article • Thrombectomy
Stroke is a surgical disease!
They did it for heart attacks. Can cardiologists now lead an effort to speed up the emergency medical response for stroke? Over the past five years, the Stent for Life initiative organised by interventional cardiologists has pushed majors medical centres to assure 24/7 coverage and reduce the time to treatment for patients showing up with severe chest pain.
Report: John Brosky
Now armed with fresh evidence that a mechanical intervention to pull out blood clots is more effective to halt devastating damage to the brain than the slower treatment with drugs to dissolve the clot, the European Association of Percutaneous Cardiovascular Interventions (EAPCI) has formally issued a call to action to mobilise its growing army of interventional cardiologists. ‘We need to build healthcare systems for early intervention in stroke,’ Jean Fajadet MD, the outgoing president of EAPCI.
Qualified physicians are needed
Even a quick glance at the number of interventional neuroradiologists in Europe compared to the number of stroke patients shows there are far too few qualified physicians to offer such a service everywhere, all the time. ‘To offer this intervention rapidly, the question becomes whether cardiologists can help,’ suggested Kenneth Snyder MD, from the State University of New York in Buffalo, who joined Fajadet at EuroPCR 2015 in calling for next-generation stroke centres.
A consensus statement issued 2015 by the European Stroke Organisation (ESO; Basel, Switzerland) unequivocally recommends rapid percutaneous intervention within 4.5 hours with a clot retrieval device.
ESO developed the statement with the European Society of Minimally Invasive Neurological Therapy (ESMINT; Zurich, Switzerland) and the European Society of Neuroradiology-Diagnostic and Interventional (ESNR; also Zurich). ‘Stroke is a surgical disease,’ Snyder declared.
‘Five clinical trials have been halted because the new technology is better'
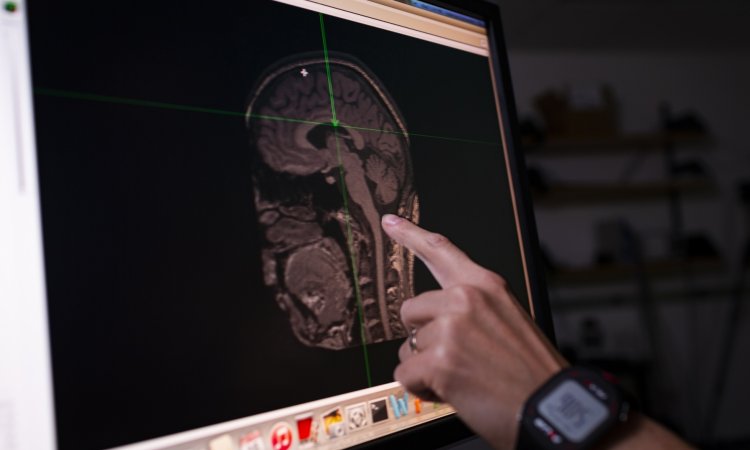
This bold statement challenges the current standard of care and is based on new scientific evidence from four major stroke studies presented this year at the International Stroke Conference in Nashville, USA. Those studies showed that rapid mechanical thrombectomy using a new generation of clot retrieval devices improves patient function after acute ischemic stroke.
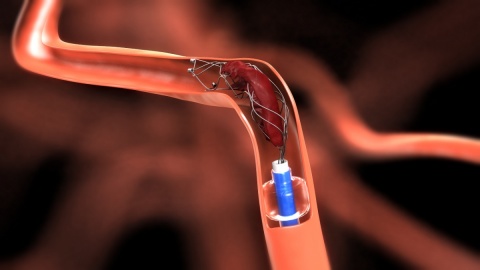
‘Five clinical trials have been halted because the new technology is better, because it works,’ said Snyder. The current standard of care for stroke patients is an intravenous (IV) injection of a tissue plasminogen activator (t-PA) meant to dissolve a clot blocking blood circulation in the brain. The new procedure for mechanical thrombectomy is a surgical intervention, in which a device is used to pull out the blood clot immediately and directly. The procedure is performed without general anaesthesia as the patient is not aware of the catheter snaking through blood vessels to arrive in the brain with a device some call simply a cork-screw.
Surgeons have reported that patients in some cases have sat up on the operating table after the clot was removed and began speaking with them. Catheter operators trained through EAPCI have the basic skill set needed for the procedure, and with additional training could maintain the 24/7 coverage for this time-critical procedure, according to Fajadet.
Membership in EAPCI has grown rapidly since it was founded in 2006. In the first five years 2,700 cardiologists joined to train for angioplasty and stenting procedures. That number nearly doubled again so that, in 2014, there were 5,500 members. There are almost 13,000 interventional cardiologists attending EuroPCR events in 2015. New devices that are generating the excitement surrounding this procedure include the Solitaire revascularisation device from Covidien and the Trevo from Stryker Neurovascular.
31.08.2015