Secondary healing wounds
Clinical success with autologous thrombocyte gel transfer*
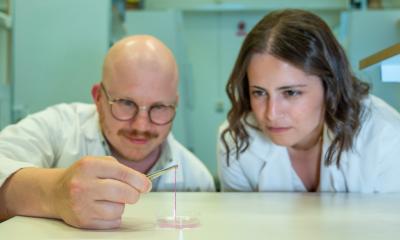
An application report by assistant plastic surgeon Thomas Aigner, and F Weyer, of the Department of Plastic, Aesthetic and Reconstructive Surgery, at St. Polten Hospital, Austria

Seemingly harmless wounds that nonetheless do not heal are a common problem in any hospital. Such wounds can turn into major problems requiring years of treatment.
Autologous thrombocyte gel has helped to heal some chronic wounds. In a new procedure, presented below, the thrombocyte gel is applied directly to the stagnating chronic wound. This leads to a concentrated release of thrombocyte growth factors (see box), which is supposed to accelerate wound healing. We analysed this procedure for clinical suitability and preliminary results, in 30 patients suffering poorly healing, split-thickness skin graft donor sites or split-thickness skin grafts.
- platelet-derived growth factor (PDGF)
- transforming growth factor beta 2 (TGF b2)
- insulin-like growth factor (IGF)
- epidermal growth factor (EGF)
- epithelial cell growth factor (ECGF)
- and many known and unknown factors.
The most important growth factors released by activated thrombocytes
All cases involved secondary healing of split-thickness skin graft donor sites, or defects of split-thickness skin grafts, which had been present for over a year and had not shown any healing progress. Despite intensive conservative therapy, optimised diet and precise neurological and internistic examination the wounds had not closed.
Procedure - 50 ml blood samples were drawn from each patient. Using an Autologous Platelet Separator thrombocyte gel (PRP) - plasma rich in thrombocytes (412000/ml - 2114000/ml) - was generated. The thrombocytes were activated with glass fibre coated with calcium chloride which triggered the release of growth factors. Then they were applied to the wound, which had been cleansed with NaCl 0.9%. For 24 hours the wound was covered with foil. The subsequent treatment was identical to the one prior to the thrombocyte application.
Results - Within, at most, four weeks each patient’s wound showed clear granulation and epithelisation. After three months, in 60% of patients the wounds had entirely closed. After application of the autologous thrombocyte gel healing and epithelisation visibly accelerated and exudations, as well as pain, were noticeably reduced. There were no complications that could have been attributed to the autologous substance.
Summary - There is currently no literature that assesses this new procedure. Therefore, it needs evaluation in clinical studies and indications should be defined. In view of the very positive results, and simple handling of thrombocyte gel, this is now established procedure in our hospital and we are about to test it in other areas.
* Based on a presentation at the Wound Management Meeting of the Academy for Wound Management Certification - Kammerlander WFI from 3-6 May 2006 in Lengenfeld, Otztal, Austria.
01.07.2006