Article • MRSA and refugees
Screening, isolation, hygiene equal money well spent
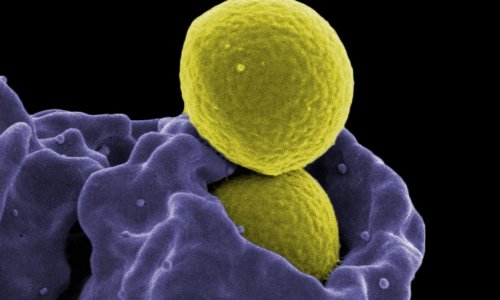
Comprehensive examinations of 143 refugee patients hailing mostly from Afghanistan and Syria, which were conducted between June and December 2015, showed a high prevalence of MRSA, ESBL and MDRGN upon hospital admission. The figures exceed not only those of the general population but, alarmingly, also those found in high-risk groups, such as residents of nursing homes or home care service patients.
Professor Ursel Heudorf of the Department of Infectiology and Hygiene at the Public Health Office in Frankfurt, Germany, is therefore demanding general screening of refugee patients upon hospital Admission.
Data speak the truth

In the population at large, MRSA rates are below one percent. Among groups at risk, such as nursing home residents, it is six to nine percent. However, among the refugee patients examined in the Rhine-Main region 9.8 percent carried MRSA. -Found to be present in approximately eight percent of the general population, these organisms were detected in risk groups between 7.5 percent (dialysis patients), 14 percent (patients of home care services) and 18 to 27 percent (nursing home residents).
During the above-mentioned study the organisms were present in 23 percent of the refugee patients, with 1.8 percent carrying MDRGN bacteria, resistant to four classes of antibiotics. Thus, refugee patients present a more severe health threat for themselves and others than the typical at-risk groups in Germany, even though the patients were primarily young and presumably without an extended history of hospital stays. ‘The result was surprising and warrants a re-evaluation of this patient group,’ says Professor Ursel Heudorf, Public Health Physician and Director of the Hygiene Department at the Public Health Office in Frankfurt/Main, Germany. While elderly people stay in hospital frequently and are treated with antibiotics, they have always been considered an at-risk group and undergo suitable hygiene procedures, refugee patients only now have been understood to be on a similar risk level and require corresponding hygiene measures.
Questioning why
Why such a large prevalence of MDRO? Heudorf assumes one reason to be ‘improper antibiotics management in the countries of origin of the refugees’. The lack of product quality assurance in the countries of origin, where antibiotics are frequently sold over the counter and might contain a lower concentration of active ingredients, might be one factor; costs might be a second one. Since the pharmaceuticals are freely available on the market they may be taken as long as they can be afforded. This may lead to antibiotics therapy being stopped prematurely since the patients subjectively feel better. ‘There are several conditions that promote resistance,’ Heudorf concludes.
Evidence-based recommendation
Medical history-based Tests? Too complicated, too error-prone
Ursel Heudorf
Therefore, she considers it ‘important to screen all refugee patients upon hospital admission’. Even the Robert Koch Institute (RKI), which previously recommended tests only if warranted by the individual patient’s medical history, now also supports screening for MRSA and 4MDGRN upon hospital admission. Medical history-based tests are difficult to implement in practice, as Heudorf points out: ‘Too complicated, too error-prone. Due to language problems on both sides, the validity of the information provided is questionable. Thus, systematic screening and initiation of hygiene measures should be performed regardless of the information provided by refugee patients during anamnesis. Heudorf is well-equipped to master future challenges. ‘Our study in the Rhine-Main area was prompted by the lack of knowledge on our new and relevant patient group – refugees. The results allow us to design an evidence-based approach.’
Preventive isolation
Depending on the procedure, each test will cost between three and 50 euros. The gold standard remains the culture on a petri dish. PCR is faster, but provides rather too many false positives. Heudorf recommends preventive isolation even before the test results are available, to be able to decide on the next steps based on results. Isolation, however, means more costs both in terms of time and human resources, for example changing times for staff. Isolation also requires more space, since only one bed can be used per room. However, financial considerations notwithstanding, Heudorf is convinced that ‘if an outbreak of multi-resistant pathogens is to be prevented in a hospital, in the end money spent on screening, isolation and hygiene is always money well spent.’
Profile:
Professor Ursel Heudorf MD, Public Health Physician and Deputy Director and Director of the Hygiene Department at the Public Health Office in Frankfurt/Main, Germany, is an expert in hygiene in medical and community facilities with a focus on multi-resistant organisms. She initiated and today heads the MDRO (Multi Drug Resistant Organism) Network Rhine-Main, which offers a wide range of services for the general public and an expert audience – such as studies on MDRO prevalence in non-acute clinical settings. The network conducted the largest multi-centre study on MDRO among refugee patients to date (all studies and further information available on www.mre-rhein-main.de).
15.06.2017