Rethink breast cancer surgery
Italian surgeon and oncologist Prof. Dr. Umberto Veronesi, Founder and Scientific Director of the European Institute of Oncology in Milan and former National Health Minister (2000 – 2001), is considered to be one of the biggest authorities on breast cancer research of our time. Many breakthrough changings in cancer medicine sustainably go back on his researches, which once earned him also a nomination for the Nobel prize. In June, Prof. Veronesi held an Honory Lecture at the 8th Duesseldorf Breast Cancer Conference in Germany about “The future of breast cancer treatment”.
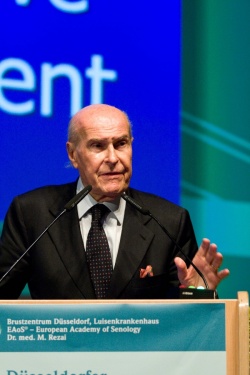
“Surgery of breast cancer more than in other tumors has gone through a number of revolutions in the last forty years, which did not so much manifest in techniques but in concepts: The rethinking from anatomical concept of cancer spread to biological concept as well as the paradigm shift from maximum tolerable treatment to minimum effective treatment are two milestones to mention,” Veronesi began his speech. Both more patient friendly concepts were essentially initiated by Veronesi himself in his Milan trials I – IV. The professor was the first to prove in a clinical trial published in 1981 that patients with small-size breast tumours undergoing a quadranectomy (quadrant resection flanked by radiotherapy and axillary dissection) have the same recovery chances like patients undergoing radical mastectomy. The results also revealed that breast cancer is a systemic disease instead of a local disease as believed in earlier doctrine which means that metastases spread from early on in the periphery. In consequence, local recurrence is not an instigator of new metastases and the survival rate at lumpectomy + radiotherapy and quadranectomy + radiotherapy is the same.
A discussion raised by the introduction of breast conservative surgery was the evaluation of margins of resection as possible predictor of recurrence. “Our Milan trials have shown that patients with negative or positive margins have the same rate of recurrence”, said Veronesi. “The evaluation of the margins is limited, because firstly, the peritumoral spread of cancer cells is often discontinuous and secondly, the biopsies on the margins of the specimen are ‘at random’. We believe that after surgery some cancer cells remain in the breast and therefore radiotherapy must be given to all patients after conservative surgery.”
In the 1990s, Veronesi began to perform sentinel node biopsy as method for screening the axillary nodes for metastasis in order to spare healthy axillary. The sentinel node is the first that receives lymph from the tumor area. So only if the sentinel node is afflicted by cancerous cells, all lymph nodes should be removed, he said. Another powerful prognostic indicator is the internal mammary node. “Mammary internal nodes are generally ignored by surgeons, but my clinical experience shows me that if axillary nodes and internal mammary nodes are both negative, the survival is good, if they are both positive, the survival is bad, and if only one of the two is positive the prognostic power is identically. In other words, the identification of the internal mammary node has the same prognostic value than the identification of the axillary node. Hence, patients with positive internal mammary nodes should receive radiotherapy to internal mammary chain and more intense systemic treatment.”
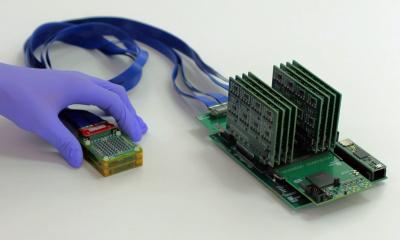
The further step to improve breast conservation was the development of ELIOT (Full Dose Intraoperative Radiotherapy with Electrons) by Veronesi. ELIOT is a focalized therapy technique to treat a more limited volume of tissue surrounding the tumour bed. A mobile linear accelerator is utilized delivering a single dose of radiation (50 Gy in three minutes) with multi-energy electrons immediately after the removal of the primary carcinoma. “The concept behind ELIOT is that local recurrences occur in 90 % of cases in the quadrant harbouring the primary breast carcinoma. So with ELIOT, we are able to pin-point the irridation on the operative field. A dedicated disk of lead and aluminium is used as a protective device. Therefore, ELIOT reduces radiation exposure to the normal tissue as well as to deep organs like the lung.” Because radiation course is shortened down from 5-6 weeks to only one session, the problem of access to radiotherapy centres, especially in rural areas, is also solved.
At the end of his lecture, Veronesi listed the most important of the novel targeted minimal-invasive treatments from his point of view:
- High-Intensity-Focused-Ultrasound (HIFU): HIFU uses high frequency sound waves to heat up small accurately-targeted amounts of tissue to a temperature of 80-90◦C. The main advantage of ultrasound in radiotherapy is the real-time guidance without requirement of surgical exposure or insertion of instruments into the lesion.
- Proton Beam Therapy (PBT): the energy that protons deliver to the tumor mass is much higher than the usual electron photon beams. While the latter go through the whole body, the irridation with protons can be controlled to stop, when it has reached the target tissue and to unfold its complete power in the tumor volume first.
- Intraoperative Avidination for Radionuclide Therapy (IART). This complex procedure consists of two steps: Firstly, the exogenous molecule Avidin is injected into and around the tumor bed during surgery. Secondly, radioactive biotin is intravenously injected into the tumor area the day after. Because Biotin shows a high affinity to Avidin, the intraoperative treatment with Avidin allows for a fast and stable uptake of the radionuclides into the tumor cells.
- Endocrine and biomolecular treatments, like drugs targeting HER2 receptor, which follow a “target and control” instead of a “search and destroy” strategy in cancer. These tumorbiological therapies allow more and more for a tailor-made, individualized treatment for the patient.
- At least, Veronesi expanded on the concept of cancer stem cells as the “root” of tumor: “Recent finding suggest that at the heart of every tumor lie a handful of malignant stem cells able to maintain the malignant tissue. In vitro and animal models have demonstrated that breast cancer stem cells are relatively resistant to both, radiation and chemotherapy. We need to change our policy of treatment and try to identify markers and membrance receptors of these cancer stem cells as targets for new drugs. For surgeons, the knowledge about presence or absence of cancer stem cells in the sentinel node biopsy could be of great help in decision making if dissection of sentinel node is needed or not.”
Text: Karoline Laarmann
26.08.2010