Article • Mid-treatment scans can reduce treatment sessions
De-escalating radiation therapy for oropharynx cancer with FDG-PET
Using fluorodeoxyglucose positron emission tomography (FDG-PET) imaging may give insights into possible dose reductions in ongoing radiation therapy of head and neck cancer. A promising study to explore this option was presented at the 2022 ASTRO/ASCO Multidisciplinary Head and Cancer Symposium held in Phoenix, Arizona.
Report: Cynthia E. Keen
Image source: Adobe Stock/Lars Neumann
Patients who have a FDG-PET scan performed two weeks into radiation therapy for p16+ oropharynx cancer may be able to have the number of treatment sessions reduced, equivalent to a 20%-30% reduction in radiation dose that can cause toxicity when delivered to sensitive structures in the head and neck. Steven G. Allen, MD, PhD, a radiation oncology resident at the University of Michigan in Ann Arbor, presented these exciting interim findings of a phase II clinical trial at the symposium. The patients who were able to receive “de-escalated” therapy experienced less toxicity and had fewer short-term side effects.
Xerostomia, a condition in which the salivary glands in the mouth do not generate enough saliva, is the most common toxicity caused by radiation to the throat. In addition to causing a very dry mouth, head and neck radiation can cause inflammation and open sores in the mouth and throat, hoarseness, loss of taste, and swallowing difficulty so severe that patients may require a temporary feeding tube. The negative impact on patients’ quality of life is significant.
Study design
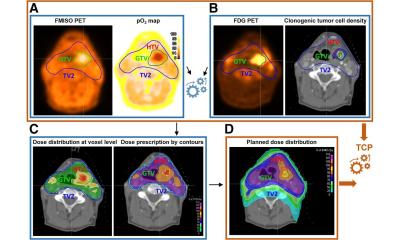
The clinical trial (NCT03829722), which is continuing enrolment of patients with stage I-II HPV-related squamous cell carcinoma of the oropharynx, is evaluating patients who show adequate tumour response after 14 days of radiotherapy treatment to determine if the number of treatment fractions can be reduced without compromising treatment efficacy. The researchers evaluate tumour response by comparing baseline and mid-treatment FDG-PET data.
Image source: Adobe Stock/Lars Neumann
In addition, principal investigator Michelle L. Mierzwa, MD, associate chair of clinical research in radiation oncology at the University of Michigan, and co-researchers will compare the percentage of patients of the standard treatment group and the de-escalated treatment group who develop local recurrence within 12 months following treatment completion, the percentage who develop cancer in any location at 24 months, and the percentage of patients who died within 24 months. The researchers are also comparing toxicity incidences at 3, 6, 12 and 24 months between the two groups.
All enrolled patients have a pre-treatment PET scan to record the metabolic activity of their tumours. In addition to receiving concurrent weekly carboplatin/pacitaxel, patients are planned to receive 70 Gy in 35 fractions. Patients who have a reduction in metabolic tumour volume greater than 50% have their radiotherapy treatment stopped at 54 Gy in 27 fractions.
Encouraging interim results
By incorporating FDG-PET scans before and midway through treatment, we have been able to adjust the radiation dose for about half of our patients to date, and to reduce their short-term side effects while still focusing on tumour control
Steven G. Allen
Dr Allen reported during the plenary scientific session presentation that 28 of the 59 patients met the de-escalation criteria. They lost less weight, a median 6% of their body weight compared to 11% for the patients who received the standard treatment. Only one patient needed a temporary feeding tube compared seven patients in the standard treatment group. They also displayed improved swallowing function on a video swallow study completed after treatment. ‘We anticipated long-term improvements in side effects, but the short-term improvements were better than expected,’ said Dr Mierzwa. ‘Experiencing fewer short-term side effects potentially allows patients to get back to their normal activities more quickly.’
‘Advanced imaging helps physicians personalise therapy based on patients’ individual tumour characteristics and response to treatment,’ Dr Allen said. ‘By incorporating FDG-PET scans before and midway through treatment, we have been able to adjust the radiation dose for about half of our patients to date, and to reduce their short-term side effects while still focusing on tumour control. Rather than completely replanning radiation treatment plans, we just stopped the treatment earlier. We are hopeful that the de-escalated treatment will be as effective at controlling the cancer as the standard treatment prescribed,’ he concluded.
29.11.2022