Radiation: How dangerous is it really?
By Dr Soenke Bartling
Radiation can't be seen or felt; it has no smell and our senses can't feel it — still it can cause great harm. Therefore, many fears are associated with radiation.

Radiation is used for diagnostic and therapeutic purposes. As with many treatments the amount of dosage is what matters. Harm from radiation can be divided into two groups, which are both present if one receives a certain amount of radiation:
1. Deterministic effect means that every exposure to a certain amount of radiation causes the same reactions. Deterministic effects are strongly dose related. Skin rash, skin burns, hair loss, bone marrow degeneration, radiation sickness and death – can be caused by a certain well-known amount of radiation. Compare deterministic effect to placing a finger on a hot plate – at a certain time and temperature you will have red skin, burn blisters and serious burns. Deterministic effects are more or less relevant for radiation therapy; here deterministic effects limit the amount of radiation that can be used to treat a patient. Cancer does not play a role in deterministic effects.
2. Stochastic effects are different. Stochastic effects of radiation cause cancer. However, it is not the case that everyone who gets exposed to radiation develops cancer – just the likelihood of cancer increases. The relation between dosage and amount of additional cancer was calculated by witnessing the survivors of atomic bombs. From the witness linear dependency we developed the theory that ever so little bit of radiation increases the risk of cancer. It might be that this view is overcautious and that the little radiation we deal with in medicine is less harmful. However, it is better to play it safe.
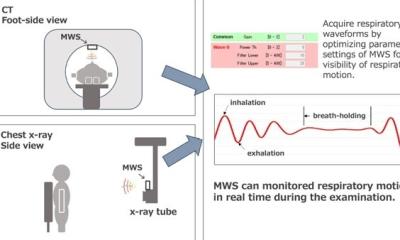
In diagnostic imaging stochastic effects are the limiting factor. Every procedure that involves X-rays increases the cancer risk of an examined patient – strictly speaking. The question here is only how much the cancer risk is increased; this can vary a lot, because the exposure caused by modalities varies in order of magnitudes. A standard X-ray exposes a patient 100-500 times less to radiation than a CT examination. Furthermore, even CT scan protocols differ in orders of magnitude with respect to patient exposure.
To give some numbers – be aware that CT scans can be very different – a CT scan that is used to rule out a pulmonary embolism causes ten cancer deaths in 10,000 people – whereas 2,500 would die of cancer anyway. While at first glance this looks like a high number, it relates well with the number of people saved by the early and right diagnosis of pulmonary embolism.
Furthermore, another factor is the patient and his/her life expectancy. For young patients radiation exposure is especially critical, while old patients are less likely to witness a consequence through radiation.
Like many things in medicine, something that helps can also harm. It is as wrong not to use an imaging modality as to use it without good reason. A specialist must decide when a diagnostic method is appropriate and when not, based on best knowledge and guidelines.
In recent years, diagnostic imaging has witnessed advances to reduce radiation: diagnostic information increased, while necessary radiation decreased.
01.11.2008