Article • Power in Hybrid
PET/MRI – powerful diagnostic tool improving with corrections
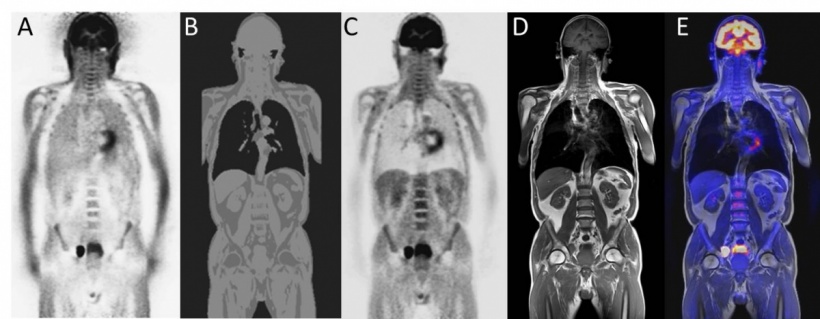
PET/MRI scanners have great potential because they combine the strengths of two different systems. Previous problems resulting from respective, mutually exclusive physical effects of both procedures have been resolved. Now these scanners are being introduced to the hospital and assist in the detection of the position and spread of tumours as well as their metabolic activity, says Dr Harald H Quick, Professor for High-Field and Hybrid MRI Imaging at Duisburg-Essen University.
Report: Sascha Keutel

PET has high sensitivity. The system can locate and measure the very smallest amounts of radiotracers in tumours and metastases and it also makes it possible to quantify their activity. ‘This is important because it allows us to classify and differentiate different tumours based on certain thresholds,’ Professor Quick explains. ‘PET also allows us to monitor a therapy after the initial diagnosis and start of treatment and shows how the activity of cell lesions develops over time and whether or not the treatment is having the desired effect.’
To fully utilise PET strengths, attenuation correction (AC) is needed. This correction is carried out by software that, in turn, is based on a mathematical solution automatically implemented by the scanner. To make this work, you need to know exactly where in a patient’s body photons attenuate in the tissue on their way to the PET detector, and then it becomes possible to calculate the AC and thus determine the correct tracer activity in the tumour. To date, AC is still required for all PET/CT hybrid systems – however, with the advantage that the raw data of CT imaging can be directly utilised for the AC of the patient tissue. However, with PET/MRI, AC must be performed with new MRI-based procedures. At the centre of this development are the Dixon method sequences, currently experiencing a revival in the context of MRI-based attenuation correction procedures. The procedure involves the attribution of different levels of attenuation to different types of tissue (air, fat, soft tissue, bone). ‘We know topographically – similar to maps – which types of attenuating tissues are in which place. ‘This can then be utilised in 3-D to work out the patient’s attenuation correction,’ he explains.
Although this works well, and is already integrated into clinical routine, room remains for improvement. With the help of comparative examinations, Prof. Quick and team are trying to determine how well MRI-based AC works compared to CT-AC. ‘Bones attenuate the PET signal comparatively strongly. The attenuating components of bones are not very visible in the MRI image and therefore cannot be adequately corrected,’ he explains.This could change with the help of ultra-short TE pulse sequences (UTE), i.e. ultra-short echo time sequences. These facilitate the detection of cranial bones in the head and therefore improve the information on brain activity quantification. ‘We have thus created the opportunity to add another dimension to the above mentioned maps,’ Prof. Quick explains, significantly adding: ‘If, in the future, we want to look at the Alzheimer tracer distribution in the brain, it will be important to account for the bones as such (and not soft tissue as is currently the case) so that we can determine activity more precisely.’
Technical pitfalls
Further technical obstacles that PET/MRI scanner manufacturers must overcome are the materials used. As is common in MRI imaging, RF receiver coils are used.These coils are within the field of the PET detector while the PET and MRI data are being acquired, and they attenuate the PET signals accordingly. Therefore, manufacturers should design the RF receiver coils in a way that makes them as PET-transparent as possible. This applies to the materials used, plus distribution and the design.
Manufacturers and researchers hope to integrate the motion correction in its entirety into the examination procedure. The PET/MRI data are currently acquired independently and simultaneously, but more or less side by side. The objective is to utilise the technical opportunities of MRI imaging, to detect the patient’s head, respiratory and heart movements and to correct the PET data helped by this information on movements – i.e. to achieve a more precise image of the moving organs, tumours or smaller lesions.
25.03.2015