Pay-for-performance bites deep
Although nosocomial infections and medical accidents have declined, over 750 hospitals with the highest number of such cases now face penalties – amounting to an estimated $330 million a year – issued by Medicare.

The Hospital-Acquired Condition (HAC) Reduction System, created as the third of the federal 2010 health law’s major mandatory pay-for-performance programmes for hospitals, levies penalties against hospitals with high readmission rates. In the second system, bonuses or penalties were based on 12 top quality measures.
However, in 2012, one in eight in-patients countrywide fell victim to a complication considered avoidable, according to a US government estimate.
Yes, infection cases are decreasing. However, their drop is less than the targets set by healthcare officials. Additionally, the appearance of new antibiotic-resistant bacteria that are considerably harder to combat, is causing more concern.
Last April, in a preliminary evaluation, federal officials identified 761 hospitals that show unacceptably high levels of these problem cases. It has been reported that this list may grow longer, given that Medicare will examine overall performances over a longer period.
This autumn, around 25% of US hospitals showing the worst infection or medical accident rates will be penalised by having to reduce each Medicare reimbursement by one percent for one year; and, with the three programmes in place, hospitals might lose as much as 5.4% of their Medicare reimbursements.
Over the first year, Medicare will observe three issues –
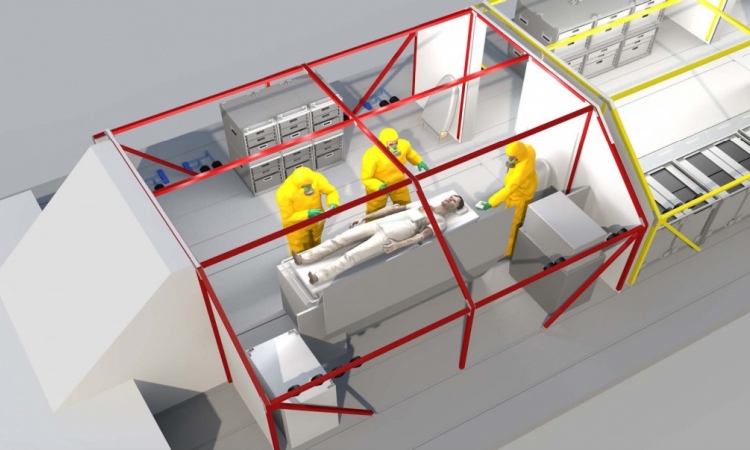
• The frequency of bloodstream infections among patients catheterised into a main artery to deliver antibiotics, nutrients, chemotherapy or other treatments.
• The cost of infections from bladder catheterization to drain urine.
• Potentially avoidable adverse conditions, such as bedsores, hip fractures, blood clots and accidental lung punctures.
Assessments are to be based on infections in 2012 and 2013.
Finally, avoidable patient safety problems that occurred from July 2011 to June 2013, including bedsores, hip fractures, blood clots and accidental lung punctures, will be included.
Over the next few years, Medicare will also consider infections in surgical wounds and the ultimate costs of infections by Clostridium difficile and methicillin-resistant Staphylococcus aureus (MRSA).
Dr Ashish Jha, a professor at the Harvard College of Public Wellness, carried out an analysis of the preliminary penalties for Kaiser Overall health News. Prof. Jha discovered that publicly-owned hospitals and those that treat large numbers of low-income sufferers are far more likely to be face penalties, as are huge, urban hospitals or those n the West or Northeast.
Medicare records reveal that preliminary penalties were assigned to far more than a third of hospitals in Alaska, Colorado, Connecticut, the District of Columbia, Nevada, Oregon, Utah, Wisconsin and Wyoming.
Surprisingly, 54% of the nation’s significant teaching hospitals were listed for preliminary penalties, according to Prof. Jha.
Clearly hospitals must decrease avoidable harm to patients and therefore costs. In 2008 Medicare began to refuse hospital reimbursement for the care of in-patients who had suffered avoidable complications.
03.07.2014