Article • Imaging modalities for quantifying myocardial blood flow
Nuclear cardiology – a nuclear perspective on matters of the heart
Nuclear cardiology is a specialised field in nuclear medicine that evaluates the heart function to help diagnosing conditions such as coronary artery disease and to assess treatment efficacy, whilst minimising invasive procedures like biopsies. More recently, clinicians have increasingly opted for nuclear imaging over endomyocardial biopsy to diagnose cardiac amyloidosis, allowing for earlier detection of the disease.
Article: Cornelia Wels-Maug

Image source: Patrick J. Lynch, medical illustrator; C. Carl Jaffe, MD, cardiologist, Heart spect imaging, CC BY 2.5
Myocardial perfusion imaging (MPI), essential in assessing blood flow to the heart muscle, plays a critical role in identifying coronary artery disease and requires scans for accurate diagnosis. While positron emission tomography (PET) is the gold standard for myocardial blood flow (MBF) quantification, the limited availability of PET scanners has led to growing interest in single-photon emission computed tomography (SPECT) as a viable alternative, though further validation and standardisation are necessary. The future of nuclear cardiology looks promising with advancements in radiopharmaceuticals, such as the recently FDA-approved F18-Flurpiridaz, and the integration of artificial intelligence to streamline quantitative assessments in cardiac PET-MPI.
What is nuclear in cardiology?
Nuclear cardiology is a subspeciality of general cardiology that evaluates how organs function. Unlike conventional imaging methods like X-rays, magnetic resonance imaging (MRI) or computed tomography (CT), which primarily visualise the physical structure of tissues and organs, it captures a wide range of metabolic processes.
Using radioactive substances that are administered in extremely small quantities and, as a rule, hardly differ from the substances naturally occurring in the organism, the function of organs, tissues and bones examined is practically not affected, but only observed. Nuclear cardiology can help to evaluate, diagnose and treat heart conditions in a noninvasive way and therefore avoids potential risks associated with a biopsy.
Nuclear cardiology imaging tests are used to determine respectively monitor:
- whether a patient’s heart-related symptoms are due to coronary artery disease or atherosclerosis
- if there is adequate blood flow to the heart muscle during stress versus rest. A restricted blood flow from the left ventricle to the aorta, for example, can lead to increased pressure in the heart and reduced oxygen supply to the body. This is called an aortic valve stenosis, a medical condition characterised by the narrowing of the aortic valve opening
- whether a person is at risk of a heart attack and needs angioplasty or coronary artery bypass graft (CABG) surgery
- a patient’s condition after CABG surgery or a cardiac catheterisation procedure
- establish the presence along with the severity of prior heart attacks (size and location) as well as the risk of future heart attacks
- evaluate how well a heart is pumping, which could indicate cardiomyopathy, heart injury or an infection
- the effects of chemotherapy or medications on a patient’s heart.
This information will help clinicians to decide more accurately on the most appropriate treatment options to take.
Nuclear imaging challenges endomyocardial biopsy
Nuclear imaging as an alternative diagnostic approach has become more popular among clinicians who suspect cardiac amyloidosis in their patients rather than performing an endomyocardial biopsy (EMB).1 Cardiac amyloidosis is a protein-folding disorder that can result in heart failure. Amyloid can be formed from many different precursor proteins, with the most common ones in the cardiac field being immunoglobulin-derived light chains – causing AL amyloidosis – and transthyretin (TTR) proteins – causing ATTR amyloidosis.1 Differentiating these two forms of cardiac amyloid is vital in determining prognosis and treatment of the disease. Doing so with nuclear imaging scans has led to earlier detection of the disease.
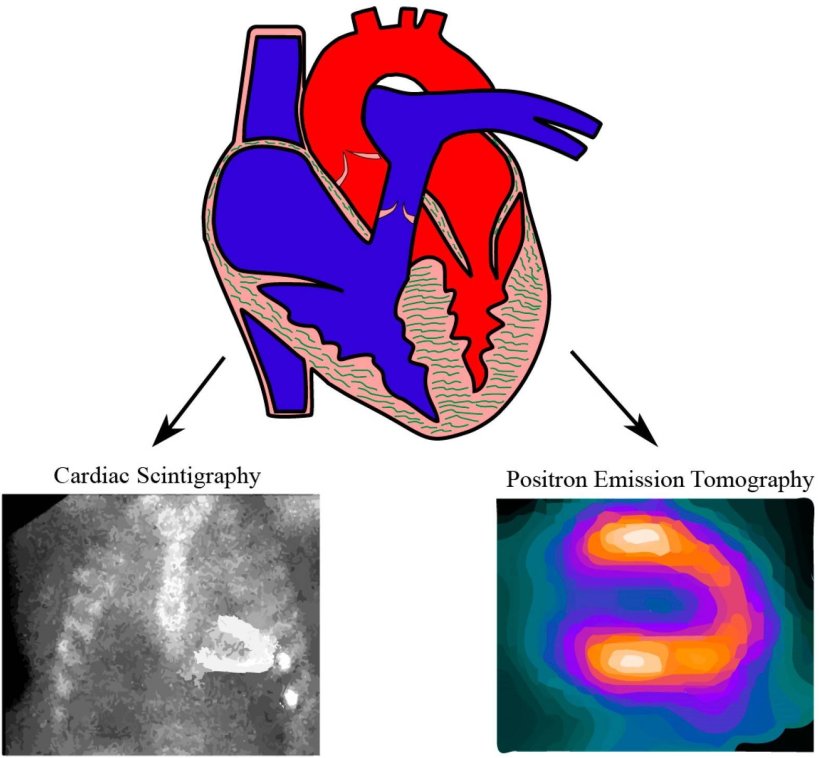
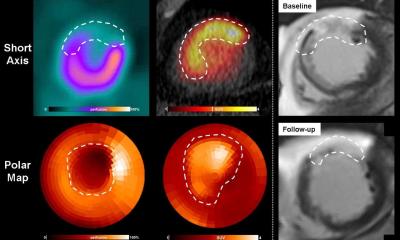
Image source: Li W, Uppal D, Wang YC et al., Diagnostics (Basel) 2021 (CC BY 4.0)
Until recently, endomyocardial biopsy was “considered the gold standard for diagnosing cardiac amyloidosis and differentiating amyloid subtypes, but its use is limited because of the invasive nature of the procedure, with risks for complications and the need for specialized training and centers to perform the procedure. Radionuclide cardiac imaging has recently become the most commonly performed test for the diagnosis of ATTR amyloidosis but is of limited value for the diagnosis of AL amyloidosis,” are the findings of a 2021 publication that investigated the role of nuclear imaging for the diagnosis of cardiac amyloidosis. The authors of the study expect that diagnosing cardiac amyloidosis with PET will expand in the future, supported by imaging protocols being under refinement to achieve better quantification of the disease burden and prediction of prognosis.
Myocardial perfusion imaging at the core of nuclear cardiology
MPI, also known as a nuclear stress test, is the most widely performed procedure in the field of nuclear cardiology. It assesses how well the blood flows to the heart muscle to diagnose and evaluate coronary artery disease (CAD). The latter occurs when the arteries supplying blood to the heart become narrowed or blocked. This clinically important assessment of cardiac function and amount of heart muscle at risk allows cardiologists to identify patients who need further testing or require medical procedures.
Using those dilaters substances creates different physiological responses than during exercise during which most patients actually experience their symptoms. More research needs to go into this
Tim P. van de Hoef
A myocardial perfusion scan is performed, for example, after a heart attack to identify areas of damaged heart muscle. Typically, MPI requires two scans — one at rest and one during exercise (walking on a treadmill or riding a stationary bike). Patients with mobility issues can be given an infusion of an intravenous pharmacological stressing agent like regadenoson, dipyridamole or adenosine. The scans reveal, which regions of the heart are healthy or injured: Areas that have absorbed the tracer are considered healthy, whereas those that have not absorbed the tracer can be regarded as damaged or lacking in good blood flow. In this context, Prof Tim P. van de Hoef, MD, PhD, Interventional Cardiologist, University Medical Centre Utrecht, the Netherlands, pointed out at the annual congress of the European Association of Nuclear Medicine (EANM’24) the results of recent studies assessing the physiology of myocardial blood flow using pharmacological agents to stress the coronary system: “We know from extensive studies in animal experiments and more recently in human studies that using those dilaters substances creates different physiological responses than during exercise during which most patients actually experience their symptoms. More research needs to go into this.”
Physiological aspects of myocardial blood flow
Van de Hoef also shared some helpful background on the physiology of MBF: “The metabolic demand of the heart increases when we exercise, primarily via an increase in the heart rate; with the rise in metabolic demand primarily accommodated through an increase in myocardial blood flow.“ This increase in blood flow is primarily generated through a decrease in microvascular resistance, he said. Van de Hoef pointed out a healthy heart’s ability of autoregulation, which he described as the “ability of the heart to maintain a constant flow in the face of a change in perfusion pressure whilst the myocardial metabolism remains unchanged.” Van de Hoef added: “Eighty percent of increase in oxygen supply to the heart muscle upon exercise is determined by an increase in coronary flow and only 20% in increase in oxygen extraction.” Referring to a meta-study that included 59,740 individuals, van de Hoef emphasised that a reduction in coronary flow reserve was strongly associated with an increase in mortality and a rise in major adverse cardiovascular events. He remarked: “Pathological changes in all compartments of the coronary circulation can lead to depletion of reserve vasodilator capacity.”
Quantifying myocardial blood flow with PET or SPECT?
Multiple nuclear imaging modalities may be used to perform an MPI. They all have in common that they are preventative and minimal invasive techniques used to diagnose and assess heart conditions. Using nuclear stress tests to determine the medical condition of a heart is an essential step to take before deciding which method of medical treatment is indicated. However, the nuclear stress test can be performed using different nuclear imaging modalities. At EANM’24 in Hamburg, a particular focus was around the performance of PET/CT and SPECT for performing MPI. Both PET/CT and SPECT are effective in evaluating blood flow. However, PET is still regarded as the reference standard for flow quantification, said Dr Laetitia Imbert, PhD, Medical Physicist, University Hospital CHRU Nancy, France. However, the number of PET scanners in Europe is not sufficient to cover the request for PET scans, remarked Prof Wanda Acampa, Assistant Professor, Federico II University Hospital, Naples, Italy. She also added that this could be a crucial driver for a shift from PET to SPECT for clinical use in nuclear cardiology as PET scanners are hardly used for cardiological imaging, but rather for oncological scans.
It is more and more interesting to try to quantify the myocardial blood flow using SPECT systems. SPECT is more widely used for myocardial perfusion imaging
Laetitia Imbert
Given the limited capacity of doing PET-MPI scans in Europe, especially in the field of cardiology, researchers explore the role of SPECT-MPI as an alternative, an area Imbert has been working on: “The quantification of myocardial blood flow with PET it is already well validated with the cardiac PET tracers 82Rb,13N, 15O-water. But there are some potential advantages of SPECT imaging, including the better availability of SPECT cameras in comparison to PET cameras.” Imbert also said, tracers for PET perfusion were expensive and not widely available unlike the tracers used for SPECT that also come at lower costs. “It is more and more interesting to try to quantify the myocardial blood flow using SPECT systems. SPECT is more widely used for myocardial perfusion imaging”, Imbert remarked.
The quantification of MBF with SPECT could be potentially useful, especially for patients with severe coronary artery disease. For performing dynamic SPECT imaging, it needs multidetector systems with fast acquisition of dynamic data in 5-10 sec, but also a tracer with a high enough myocardial flow extraction fraction at high flow rate, as well as advanced reconstruction methods. “With the dynamic acquisition and dynamic reconstruction, we will have many frames with a short time acquisition, and this will increase the noise in the reconstruction. The development of models, algorithms and data processing methods will become increasingly important to enable dynamic SPECT with a good kinetics analysis but also to obtain accurate results,” Imbert explained. She also added that for the quantification of MBF with SPECT, the focus had switched to cadmium zinc telluride (CZT) solid- state systems with dedicated cameras to perform cardiac investigations and more recently to whole-body 360-degree CZT systems. These CZT cameras facilitate the determination of MBF due to their higher sensitivity compared to the conventional SPECT, resulting in higher image quality and an enhancement in the spatial resolution (which is linked to the pixelated size of pixelated detectors). Imbert concluded: “PET is still the reference standard for flow quantification, but CZT SPECT is an alternative for flow quantification although further validation work is required before full clinical acceptance.” She pointed to the large variability among dynamic cardiac SPECT imaging in the literature with regards to variations in the acquisition duration and temporal framing, algorithms used for the image correction and reconstruction in addition to some discrepancies related to the post-processing. She urged: “Standardisation is required to achieve reproducible and accurate quantification.”
Outlook
The expected growth of radiopharmaceutical options for PET in the near future promises to rapidly expand access options to PET-MPI and likely reduce the costs of PET-MPI.
The introduction of the novel PET-MPI agent F18-Flurpiridaz, which recently gained approval by the U.S. Food and Drug Administration (FDA), is seen as a positive sign for the growth of PET-MPI. It is the first new radiotracer for nuclear cardiology for use in adult patients with known or suspected coronary artery disease to evaluate for myocardial ischemia and infarction in nearly three decades. Furthermore, many of the challenging quantitative tasks for cardiac PET-MPI will continue to be simplified and automated by using artificial intelligence.
Reference:
- See Li W, Uppal D, Wang YC, Xu X, Kokkinidis DG, Travin MI, Tauras JM. Nuclear Imaging for the Diagnosis of Cardiac Amyloidosis in 2021. Diagnostics (Basel). 2021 May 30;11(6):996. doi: 10.3390/diagnostics11060996. PMID: 34070853; PMCID: PMC8228334. https://pmc.ncbi.nlm.nih.gov/articles/PMC8228334/
This article was originally published by the European Association of Nuclear Medicine (EANM) as part of The Hamburg Collection, a set of articles highlighting key themes presented at the EANM’24 Congress in Hamburg. Republication kindly permitted by the EANM.
24.02.2025