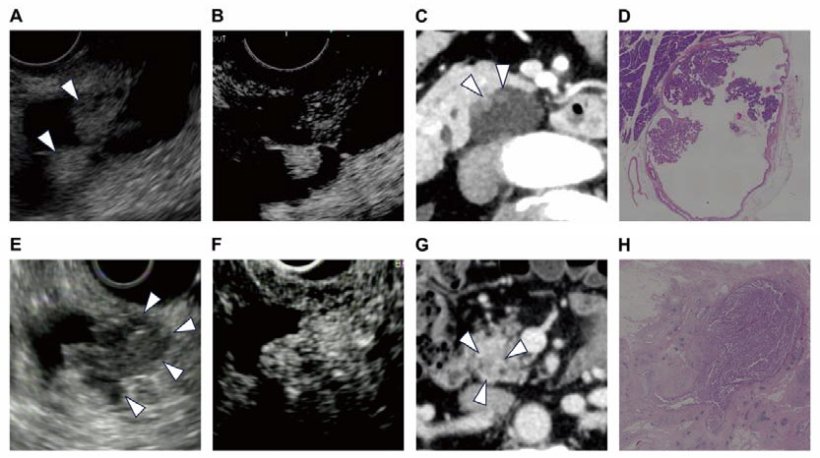
Invasive nodule: (E) EUS shows the nodule in the cystic lesion, invading the pancreatic parenchyma, and showing no clear boundaries of the cyst wall. (F) Contrast enhancement was detected in the lesion on CE-EUS. (G) On the CT portal phase (0.5 mm slice), an obscure nodule with a contrast effect is shown. (H) Histological sections showing invasive Intraductal Papillary Mucinous Carcinoma invading the pancreatic parenchyma.
Image source: Kumano R, Ohno E, Ishikawa T et al., Annals of Surgery 2025 (CC BY-NC-ND 4.0)
News • Prognostic role of IPMNs
Nodules key to avoid unneccessary pancreatic cancer surgery
Pancreatic cysts are fluid-filled sacs that can form in the pancreas. Some remain benign, while others have the potential to develop into pancreatic cancer.
A recent study, which followed 257 patients in Japan for an average of five years, showed that the presence or absence of invasive nodules in pancreatic cysts is key to assessing whether these cysts are benign or cancerous. The findings, published in the journal Annals of Surgery, may help patients diagnosed with a high risk of pancreatic cancer to avoid unnecessary surgery.
Pancreatic surgery is a significant burden for patients, so we wanted to find a more accurate way to diagnose whether their IPMNs are benign or cancerous in order to avoid unnecessary surgery
Ryohei Kumano
Pancreatic cancer is one of the most life-threatening and rapidly growing cancers. Pancreatic cysts, known as pancreatic intraductal papillary mucinous neoplasms (IPMNs), are gaining attention as one of the precursors of the cancer that can be identified by radiological imaging. In this context, patients diagnosed with pancreatic cysts are referred for further evaluation, and if they meet the criteria for being at particularly high risk of developing cancer, called high-risk stigmata, they are often recommended for surgery.
However, it was not clear whether all patients who met the criteria would need to undergo surgery. “In fact, among patients who underwent surgery, there were a number of cases where pathological examination results showed that their IPMNs were still benign and had not progressed to cancer,” explained Ryohei Kumano from Nagoya University, the first author of the study. “Pancreatic surgery is a significant burden for patients, so we wanted to find a more accurate way to diagnose whether their IPMNs are benign or cancerous in order to avoid unnecessary surgery.”
A research group consisting of Professor Hiroki Kawashima and Dr. Kumano from Nagoya University Graduate School of Medicine, Professor Eizaburo Ohno from Fujita Health University, and their colleagues focused on the presence or absence of invasive nodules in 257 IPMN patients with high-risk stigmata. The researchers evaluated the prognosis of the patients with and without these nodules.
Invasive nodules, solid growths within cysts that have begun to invade surrounding tissues, are difficult to detect with a conventional method that uses a CAT scan. Therefore, the researchers instead used contrast-enhanced endoscopic ultrasound, which is thought to detect invasive nodules more accurately. To track the prognosis of patients with and without invasive nodules between surgical and non-surgical groups, the researchers followed them for an average of about five years (ranging from 6 months to 24 years, depending on the patient).
The results showed that the presence or absence of invasive nodules had a significant impact on their survival. For patients with invasive nodules, undergoing surgery had a positive effect on improving their survival. On the other hand, most patients without invasive nodules had a favorable outcome even without surgery.
In this study, a total of 21 patients who did not have invasive nodules opted for clinical monitoring instead of surgery. Notably, their five-year survival rates were 84.7% for overall survival and 100% for disease-specific survival. In addition, in patients at higher risk for surgery, such as the elderly, there was little difference in survival rates between patients who underwent surgery and those who did not, if they had no invasive nodules. “Avoiding surgery, especially in such patients, seems to be a reasonable treatment strategy, given the fact that pancreatic surgery is highly invasive, carries a high risk of complications, and requires a long recovery period,” Kumano said. “We expect that our findings will contribute to future clinical guidelines for IPMNs, leading to more accurate cancer diagnosis and optimized treatment selection.”
Source: Nagoya University
23.04.2025